By: Elizabeth Obigwe. Freelance Writer, with medical review and editorial support by the DLHA Team

Face of an African man with red eyes
Although comparable data are not available for African countries, about 2–3% of patient visits to the doctor's clinic and emergency facilities in the United States are for ocular complaints and the majority of these visits are for the management of the red eyes.
Red eyes are usually self-limiting and are the most common non-refractive ocular complaint requiring medical attention.
Not uncommonly though, red eyes can be a cause of concern because they are sometimes an indication of more serious eye or health problems. Also, the redness of the eyes may be accompanied by other symptoms such as tearing and pain which causes discomfort.
This article will discuss the different causes of red eyes in sub-Saharan African population. It’s treatment and prevention is the subject of another report.
Red eyes or bloodshot eyes occur when the blood vessels in the conjunctiva (the thin transparent layer covering the eyelids and the white part (sclera) of the eyes (figure 1) become larger than usual. This can happen in one or both eyes and can also appear suddenly or over time.
Figure 1: The eye showing the conjunctiva. Click on image to enlarge. Image credit: American Academy of Ophthalmology.
The different categories of causes of red eyes (conjunctivitis) are:
This is the most common cause of red eyes and it involves the inflammation of the conjunctiva.
Infectious conjunctivitis can be either viral or bacterial. Viral conjunctivitis is the most common cause of infectious conjunctivitis. It is also more common in adults than children.
Viral conjunctivitis is most commonly caused by the following classes of viruses; adenovirus, herpes simplex, and molluscum contagiosum.
In African children, Rubrola (measles) virus - a Morbillivirus - is a common early cause of viral conjunctivitis that may proceed to more serious visual complications like disfigurement (scarring) of the cornea and even blindness.
When red eyes is caused by the adenovirus, it is highly contagious, whereas that caused by the other viruses is less likely to spread.
A common form of viral conjunctivitis caused by an enterovirus occurs seasonally every rainy season in countries of the West Africa region. It is popularly referred to as "Apollo" by locals because reports of its first epidemic in Nigeria and Ghana for example coincided with the Apollo 11 moon landing in July 1969.
Viral conjuctivitis usually spreads through direct hand-to-eye contact, medical instruments, swimming pool water, or personal items. It can also be associated with upper respiratory tract infection which spreads through cough.
Keep in mind that viral conjunctivitis is self-limiting (i.e., it goes away on its own) and in most cases, does not require topical antibiotics. In severe cases, you may feel discomfort after the condition resolves. You should see your ophthalmologist.
The less frequent cause of infectious conjunctivitis is bacterial conjunctivitis. It is more common in children.
The most common bacteria that cause bacterial conjunctivitis are Haemophilus influenza, Streptococcus pneumonia, and Staphylococcus aureus.
Bacterial conjunctivitis is highly contagious and is most commonly spread through contaminated hand-to-eye contact. Based on the duration and severity of signs and symptoms, the condition can be hyperacute, acute, or chronic.
Symptoms of infectious conjunctivitis are;
Keratitis is the inflammation of the cornea. The cornea is the thin transparent membrane which lies over the front dark part of the eyes (figure 2).
Keratitis can be infectious or non-infectious. It is non-infectious when it is caused by eye injury or similar factors. Infectious keratitis may be bacterial, viral or fungal and they are usually unilateral. (i.e., affecting only one eye).
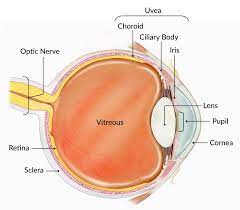
Figure 2: The eye showing the cornea. Image credit: National Eye Institute.
Bacterial keratitis hardly affects a normal eye because the membrane of the cornea provides a barrier against many organisms. Corneal ulceration mostly occurs when there is a breach of the barrier.
Conditions that can put the eyes at risk for bacterial keratitis include:
Pre-existing ocular surface disease
Contact lenses
Corneal abrasions
Physical and chemical trauma
Refractive surgery
Diabetes
Immunosuppressive diseases and
Topical steroids
Viral keratitis is mostly caused by herpes simplex virus and it is a major cause of corneal scarring globally.
Fungal keratitis on the other hand is an important cause of infectious blindness in developed countries.
Keratitis is an ocular emergency because it progresses rapidly. Hence, it requires prompt and specific management to keep the eyes safe.
Symptoms of infectious keratitis are;
Red eyes
Photophobia
Discharge
Decreased vision
Corneal edema
Corneal ulceration
Orbital cellulitis is a serious infection of the tissues surrounding the eye, including the eyelids, orbit, and neighbouring bony sinuses. It is usually caused by bacterial infections, most commonly by Staphylococcus aureus and Streptococcus pneumoniae. This condition requires urgent in-hospital treatment to prevent sight and life-threatening complications.
Symptoms of orbital cellulitis are;
Scleritis is a rare eye inflammation that affects the sclera which is the white part of the eye (figure 2). It can occur at any age, but it is most common in people between 30 and 50 years. This condition is severe, causes red eyes with pain and can lead to vision loss. It is sometimes an indication of an underlying systemic disease.
Scleritis can be infectious or non-infectious. Non-infectious scleritis is classified into anterior (front of eyes) and posterior (back of eyes). The anterior scleritis is further divided into diffuse, nodular or necrotising. It is diffuse when the redness spreads all over the eye. But if the redness appears in a part of the eyes, it is nodular. Necrotizing scleritis results in the death of tissues.
Symptoms of scleritis are;
Episcleritis is an inflammatory condition that affects the episclera. The episclera is the thin layer of tissue between the conjunctiva and the sclera. Unlike scleritis, episcleritis is mild and non-vision-threatening. The condition usually happens at intervals and is self-limiting (i.e., it goes away on its own). Although it can affect anyone, it is mostly common among young to middle-aged women.
Just as with anterior scleritis, there are diffuse and nodular episcleritis. But episcleritis is not necrotising.
Symptoms of episcleritis include;
This is a chronic eye inflammation that affects the eyelids and can cause redness, itching, and irritation of the eyes.
Blepharitis is divided into anterior and posterior. Anterior blepharitis is the inflammation of the eyelashes and follicles while posterior blepharitis involves the Meibomian glands - these are large "oil-producing" glands that line the edge of the eyelids where the eyelashes are found.
Anterior blepharitis is usually infectious. It can be bacterial (Staphylococcus), viral (Molluscum contagiosum), or parasitic (phthiriasis, demodex ). It can also cause inflammatory skin conditions such as atopy and seborrhea.
Posterior blepharitis is commonly metabolic. This condition is often associated with systemic diseases like rosacea and seborrheic dermatitis.
Symptoms of blepharitis include;
Acute angle-closure glaucoma is a medical emergency that occurs when the drainage angle between the iris and cornea becomes blocked, leading to a sudden increase in the pressure within the eye. It is one of the causes of red eyes with pain. You can read more about acute angle-closure glaucoma and other types of glaucoma here.
Symptoms of acute angle-closure glaucoma include;
Uveitis is an inflammation of the uvea or uveal tract, which is the middle layer of the eye between the visible white part and the retina behind. It is composed of the iris, the ciliary body and the choroid.
Based on the different eye parts that make up the uvea (see figure 2), uveitis can be divided into anterior (affects the iris), middle (affects the ciliary body), posterior (affects the choroid), and panuveitis (affects the entire tract). Anterior uveitis which affects the iris is also called iritis and it causes the worst red eyes.
Symptoms of uveitis include;
Allergic red eyes are usually due to irritation of the conjunctiva. There are six common causes of this type of red eye.
This is the most common allergic cause of red eyes. Its symptoms are typically seasonal and associated with native plants and grasses. The symptoms are also bilateral with itching occurring first followed by burning and tearing.
PAC is similar to SAC. However, it is more chronic in nature because the allergens are present throughout the year. It is also less severe and allergens like house dust are associated with it.
Vernal keratoconjunctivitis usually occurs in adolescent males, and it typically starts between ages eight to twelve. It is often associated with asthma, eczema or allergic rhinitis (stuffy nose). Usually, the eyes get very itchy and have a burning and foreign body sensation. You may also have photophobia and blurred vision.
Adults who exhibit other systemic symptoms of atopy are most likely to develop Atopic keratoconjunctivitis. There is also hypersensitivity to allergens most frequently linked to asthma, rhinitis, dermatitis, or food allergies.
The condition causes photophobia, discomfort, and blurred vision in addition to itchy, watery, burning eyes. AKC presents similar to vernal conjunctivitis, except that there is a chance of conjunctival scarring in conjunction with symblepharon formation.
CLPC is also known as giant papillary conjunctivitis and its exact cause still remains unclear.
Scientists say it may be an allergic response to the contact lenses themselves, contact lens solutions, the preservative in the solution, or deposits on the contact lens. It is also possible that rubbing the lens or lens deposit on a part of the upper eyelid known as the tarsus may also play a role.
CLPC is more common in standard soft contact lens wear compared to either disposable soft contact lenses or rigid gas-permeable contact lenses.
Early symptoms include blurred vision, increased mucus production, itchy eyes, enlarged papillae on the superior tarsal conjunctiva, etc.
In this condition, it is often difficult to tell if an agent caused an allergic or toxic response. The common causative agents are; ocular medications, preservatives, chemicals such as those found in cosmetics and hair spray, and other kinds of foreign body
Subconjunctival haemorrhage and corneal abrasion are some of the common traumatic causes of red eyes.
This is a common condition that occurs when a blood vessel in the conjunctiva breaks, causing blood to leak into the surrounding tissue. It can cause redness and a painless, bright red patch on the white of the eye. Causes of trauma may include a foreign body, blunt or penetrating injury to the globe, vigorous rubbing of the eyes, etc. Treatment is usually not necessary, as the condition will resolve on its own within a few weeks.
This is a scratch or scrape on the cornea. It can be caused by a foreign body or direct injury from a finger, stick, or piece of paper. It results in eye redness, pain, tearing, and sensitivity to light. Treatment may include the use of topical antibiotics, lubricants, and pain relief medication, as well as the avoidance of contact lenses and eye rubbing.
Corneal flash burn is a superficial inflammation of the cornea that occurs after extensive exposure to ultraviolet light, from welding, skiing, or a sun lamp without using protective goggles. It often causes intense pain, burning, blurred vision, watering, and blepharospasm.
Chemical burns in the African setting may include common agents such as local gin and Cow's urine eye wash. Other agents are; cement, plaster powder, oven cleaner, and drain cleaner. Alkali burns produce liquefaction necrosis of the conjunctiva and cornea, which continue to dissolve soft tissue until completely removed.
Environmental factors that cause red eyes are often related to exposure to irritants or allergens in the surroundings. In many cases, environmental causes of red eyes can be managed effectively by avoiding triggers and using over-the-counter remedies. However, if red eyes symptoms persist or worsen, or if there are signs of eye injury, it's important to consult your doctor.
These causes include;
Although we have classified the causes of red eyes into broad categories, it is important to note that sometimes, there can be overlaps between the different classifications. For instance, a causative factor can be both infective and inflammatory.
The prevalence or commonness of the different causes of red eyes can vary among regions and races.
A study carried out in Nigeria revealed that there was a 32% prevalence of allergic conjunctivitis which was similar to findings in other hospitals in Africa. However, this was different from what is obtainable among Caucasians.
1. Singh RB, Liu L, Anchouche S, Yung A, Mittal SK, Blanco T, Dohlman TH, Yin J, Dana R. Ocular redness - I: Etiology, pathogenesis, and assessment of conjunctival hyperemia. Ocul Surf. 2021 Jul;21:134-144. doi: 10.1016/j.jtos.2021.05.003. Available from here.
2. Lambert L. Diagnosing a red eye: An allergy or an infection? South African Family Practice, 2017;59(4), 22–26. doi: 10.4102/safp.v59i4.4726. Available from here.
3. Smit DP, Randall AS, Mohamed N. Basic ophthalmology for the primary healthcare practitioner: the red eye. SA Pharmaceutical Journal, 2013;80(7), 20-26. Available from here.
4. Provine RR, Cabrera MO, & Nave-Blodgett J. Red, yellow, and Super-White sclera. Springer Nature Link, 2013;24(2), 126–136. doi: 10.1007/s12110-013-9168-x. Available from here.
5. Muntingh GL, Viljoen M. (2018). A "site" for sore eyes. South African Family Practice, 2018;60(6), 7-11. Available from here.
6. Schmid KL, Schmid LM. Ocular allergy: causes and therapeutic options. Clinical and Experimental Optometry, 2000;83(5), 257-270. Available from here.
Related:
Published: October 6,, 2023
© 2023. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content without alteration or modification and subject to attribution as to source.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.