Childhood Diabetes in Sub-Saharan Africa: Type 1
By Chinonso Cynthia Ukah. BNSc, RN, RM, RPHN. Freelance Health Writer. Medically reviewed by A. Odutola, MBBS, PhD, FRCSEd.

A cute black child with her mother. Image credit: Freepik
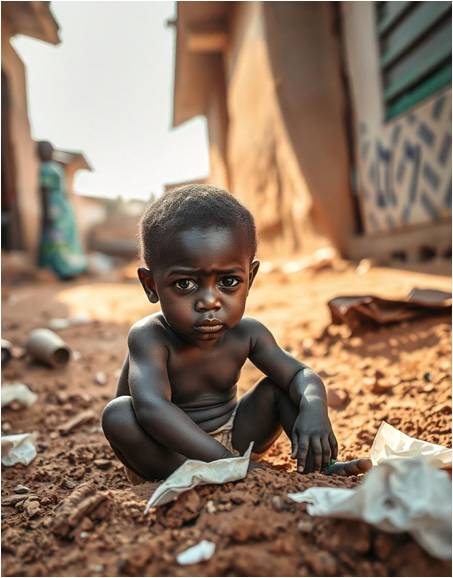
An African child. Generated with Freepik.
When childhood diabetes is mentioned, what often comes to mind is type 1 diabetes. This was previously known as juvenile and insulin-dependent diabetes.
But there are other types of diabetes that affect children under 5 and adolescents under 19. They range from type 2 diabetes (T2D),and other atypical diabetes, including malnutrition-related diabetes. [1]
Families with diabetic children in developed countries do have challenges coping with the disease, even with good access to the best treatment options and expert medical care. [1]
Across countries in Sub-Saharan Africa, where basic resources for diabetes management are often scarce or inaccessible, childhood diabetes awareness and care are more challenging.
This article aims to raise awareness and educate you about childhood diabetes. It will explore the different types that affect children in sub-Saharan Africa, ways to recognize them, how to manage and prevent them and some of the challenges facing diabetic children in the continent.
Type 1 diabetes is an autoimmune disease in which the body's defence (immune) system attacks the special cells (insulin-producing beta cells) of the pancreas, resulting in the body producing very little or no insulin.
Insulin is one of two major hormones in the body that regulates sugar level in the body.
Type 1 diabetes is mostly seen in children, although it can occur in other age groups.
According to a report, between 2011 and 2012, the Africa Region recorded a five-fold rise in type 1 diabetes among children and teenagers below 19 years, with cases surging from four per 1000 children to nearly 20 per 1000. [2]
In 2021, over 1.2 million children and adolescents globally were diagnosed with type 1 diabetes, with 59,500 of them in Africa. [3]
In light of the health system challenges facing sub-Saharan Africa, it is reasonable to suspect that the reported number of new diabetes cases may be higher than estimated because some cases are missed, and some children even die without type 1 diabetes being confirmed as the cause of death. [4]
There are several ways to recognize when your child is suffering from type 1 diabetes. These include the following:
These are some of the concerns you may have or observe:
Although not specific to diabetes, there are certain behaviour changes that you may observe in older (adolescent) children with type 1 diabetes. [5] Some of these may include:
If you notice any of the listed signs, symptoms and behaviour changes in your child, take them to see a doctor for accurate diagnosis immediately.
The diagnosis of type 1 diabetes by your child’s healthcare provider involves taking a medical history, performing a physical exam, and ordering laboratory tests including, blood and urine tests.
In taking a medical history, the healthcare provider will ask about:
his will involve:
Common blood tests that the healthcare provider may request include:
The treatment of type 1 diabetes in children can be tasking, and includes the following approaches:
The International Society for Pediatric and Adolescent Diabetes recommends 60 minutes of moderate-to-vigorous physical activity (MVPA) each day.8
As a parent, you should learn how to reduce the risk of hypoglycemia or low blood sugar in your child, promote healthy eating, physical activity, and participate in their overall diabetes management.
Children who are diagnosed with type 1 diabetes are mostly prone to developing low blood sugar (hypoglycaemia), and this occurs more often with children on insulin injections. [6]

Hypoglycemia can occur in children with type 1 diabetes. Image generated with Freepik.
Hypoglycemia is an abnormal condition where blood glucose levels fall too low such that it triggers stressful responses in the child.
Some of the indicators of low blood sugar (hypoglycaemia) in children include:
1. Palpitation: The child's heart beats faster than usual
2. Sudden and excessive sweating: Sweat appears on their forehead or palms suddenly.
3. Agitation: Their hands or body starts to shake like they're catching a cold but this is due to the low blood sugar.
4. Anxiety/Fearfulness: The child feels unusually anxious or scared, even when there's no obvious reason to be scared.
5. Sudden weight loss: The child starts to lose weight suddenly as they're not able to get nutrients into their blood cells.
6. Weakness/Fatigue: The child feels too tired to participate in their usual plays and sometimes is unable to stand due to lack of energy.
7. Mental disorientation: The child might seem disoriented, have trouble thinking clearly, or not understand what's happening around them.
8. Skin discolouration: Their skin looks unusually light or pale and loses its normal colour.
9. Sudden loss of consciousness: The child might even lose consciousness, in severe cases. [6]
If you want to reduce the negative effects of hypoglycaemia in your child, the first thing to do is perform regular blood sugar tests, especially at night.
At night, the blood glucose level usually may drop compared to daytime because of increased digestion and release of insulin and can lead to hypoglycemia if not carefully monitored.
There are effective ways to prevent and minimise the risk of low body sugar (hypoglycaemia) in your child. These include:
There is no single established way to prevent type 1 diabetes in a child at the moment. However, diabetes researchers have been actively studying and testing various ways to prevent the onset of the disease in children who have risk factors. [7]
As type 1 diabetes mellitus is an autoimmune disease where the body mistakes its healthy tissues as foreign and attacks them, the goal of prevention is to delay this process. This starts from pregnancy if you're a mother with diabetes.
After birth, other ways you can prevent type 1 diabetes from progressing in your child is to:
Type 1 diabetes in children is an autoimmune condition that requires vigilant management, which is often challenging in resource-limited regions like Sub-Saharan Africa. It can be successfully managed with regular insulin administration, careful blood sugar monitoring, proper nutrition, and appropriate physical activity. Even though it cannot be prevented, with early recognition of symptoms, consistent medical care, and strong family support, children with type 1 diabetes can lead healthy, active lives despite the challenges. Researchers are actively looking for ways to slow down the progression of the disease from its preclinical phase to the clinical and complication phases. Some of these preventive ways have been found effective in the laboratory.
1. Deeb A, Akle M, Alame M, Al Ozairi A, Abou-Ragheb L, Akle B. Common Issues Seen in Pediatric Diabetes Clinics, Psychological Formulations, and Related Approaches to Management. J Diabetes Res. 2018 Feb 27;2018:1684175. doi: 10.1155/2018/1684175. Available from here.
2. IAHO & WHO. Diabetes, A Silent killer in Africa. Analytical fact sheet. [Internet]. March 2023. [Cited 2024 Dec 14]. Available from here.
3. International Diabetes Federation. IDF Diabetes Atlas, 10th edition. Brussels, Belgium: International Diabetes Federation; 2021. Available from here.
4. Musoma SN, Omar A, Mutai BC, Laigong P. Outcomes of children and adolescents admitted with diabetic ketoacidosis at Kenyatta National Hospital (KNH), Kenya. Journal of Diabetes Research. 2020;2020(1):8987403. Available from here.
5. Litmanovitch E, Geva R, Rachmiel M. Short and long term neuro-behavioral alterations in type 1 diabetes mellitus pediatric population. World J Diabetes. 2015 Mar 15;6(2):259-70. doi: 10.4239/wjd.v6.i2.259. Available from here.
6. Gonder-Frederick L, Nyer M, Shepard JA, Vajda K, Clarke W. Assessing fear of hypoglycemia in children with Type 1 diabetes and their parents. Diabetes Manag (Lond). 2011;1(6):627-639. doi: 10.2217/DMT.11.60. Abstract available from here.
7. Ingrosso DM, Quarta MT, Quarta A, Chiarelli F. Prevention of type 1 diabetes in children: A worthy challenge?. International Journal of Environmental Research and Public Health. 2023;20(11):5962.doi: 10.3390/ijerph20115962. Available from here.
Related: Type 1 Diabetes Mellitus: An Explainer for Africans
Published: February 9, 2025
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content freely for non-commercial purposes without alteration or modification and subject to source attribution
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.