Diphtheria Explained for Africans: Causes, Symptoms, Treatment and Prevention
By Adebowale Bello. B.Tech Microbiology, Freelance Health Writer.

All you need to know about diphtheria
In 1925, a diphtheria outbreak in Nome, Alaska, United States, left an isolated town racing against time. With no access to life-saving medicine, a relay of sled dogs covered nearly 700 miles (1,127km) through treacherous winter conditions to deliver an antitoxin. This dramatic rescue was known as the "Great Race of Mercy."
Nearly a century later, diphtheria still remains a threat. The World Health Organization (WHO) reports thousands of cases annually and there have been recent outbreaks in countries like Nigeria, India and Indonesia. In Nigeria alone, more than 1,300 people have died from diphtheria since 2022, primarily children who were not fully vaccinated.
Despite medical advancements, the disease persists where healthcare access is limited and immunisation rates are low.
Diphtheria is a highly contagious germ (bacterial) infection caused by Corynebacterium diphtheriae. The respiratory form primarily affects the throat and upper airways (see figure 1), producing a toxin that can cause severe complications, including breathing difficulties, heart failure and nerve damage.
The disease spreads from person to person through droplets from coughing or sneezing, as well as direct contact with contaminated surfaces. In some cases, a person (known as a carrier) may not show signs of diphtheria but can still transmit the disease to another individual, while some others may only show mild disease symptoms. (1)
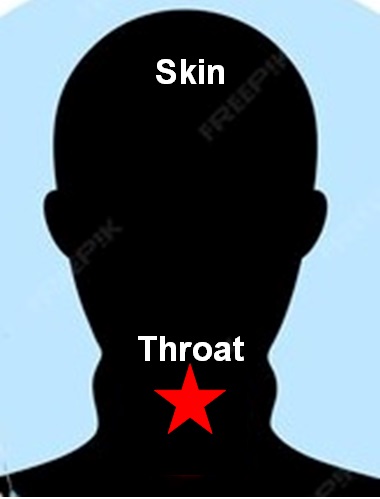
Fig. 1: Diphtheria may affect the throat and upper airway as well as the skin
Apart from respiratory diphtheria, Corynebacterium diphtheriae can also cause cutaneous diphtheria affecting the skin (fig. 1). Painful sores and blisters begin to form on the skin and it is highly contagious (2).
Although diphtheria can infect people of all ages, it majorly affects unvaccinated children under 10 years old.
For people who have been exposed to the infectious disease, symptoms develop within 2 to 5 days (1). The severity of these symptoms depends on several factors such as the individual's immune response and vaccination status.
Fig. 2: Diphtheria symptoms. Click on image to enlarge.
Here are some of the symptoms (see fig. 2) (1):
1. Sore throat: This is one of the earliest signs of diphtheria and it is often accompanied by pain and discomfort as the person finds it difficult to swallow food.
2. Voice Hoarseness: If the bacteria infect the larynx, it can affect the voice, making it rough and harsh thereby leading to difficulty in speaking.
3. Thick greyish-white membrane in the throat: This is a major symptom of diphtheria as the tough coating can cover the tonsils, throat and nasal passages, making breathing difficult (see item at black star in fig. 3).

Fig. 3: Image showing the mouth of child with diphtheria. Classic thick throat membrane is identified at black star.
4. Swollen lymph nodes: The infection causes inflammation and swelling in the neck, leading to a “bull neck”.
5. Fever and chills: A mild to moderate fever, often accompanied by general body weakness.
However, when the disease is not diagnosed on time and treated promptly, the toxin may spread beyond the throat and can cause life-threatening complications, such as:
Several factors increase the likelihood of contracting diphtheria. These factors are often linked to vaccination status, living conditions and access to healthcare (see fig. 4).
Fig. 4: Showing diphtheria risk factors. Click on image to enlarge.
The primary risk factor for diphtheria is not being vaccinated or not receiving booster doses. The diphtheria toxoid vaccine is highly effective in preventing infection but immunity wanes over time, hence booster shots are required every 10 years. Children and adults who are not vaccinated are at the highest risk of severe disease and complications.
Diphtheria spreads easily in overcrowded environments with poor sanitation. Slums, refugee camps, military barracks, schools and prisons are high-risk settings where the infection can rapidly spread through close contact and shared air (1).
Individuals with weakened immune systems, such as those with malnutrition, HIV/AIDS or other chronic illnesses are more vulnerable to infections, including diphtheria. Their bodies may struggle to fight off the bacteria or respond effectively to vaccination.
Diphtheria remains a health concern in some parts of Africa, South Asia and Eastern Europe where vaccination coverage is low. People traveling to these regions without proper immunisation are at risk of exposure.
In areas with limited access to healthcare, cases of diphtheria often go undiagnosed or untreated, allowing the disease to spread. A lack of diphtheria antitoxin (DAT) and antibiotics in some regions can also lead to severe complications and higher mortality rates.
Early diagnosis of diphtheria is critical for prompt treatment and preventing complications. A history of exposure to an infected person or living in an area with an outbreak increases suspicion. Since the disease progresses rapidly, healthcare providers often begin treatment based on clinical suspicion before laboratory confirmation.
Doctors diagnose diphtheria based on the medical history and physical symptoms, especially when a patient complains of having:
To confirm diphtheria, laboratory tests are performed, including:
In severe cases, blood tests may be conducted to check for signs of systemic infection, heart damage, or inflammation caused by the diphtheria toxin.
Diphtheria symptoms can resemble other illnesses like strep throat, infectious mononucleosis, or Vincent’s angina. Doctors rule out these conditions through lab testing and clinical assessment.
A swift diagnosis ensures that patients receive antitoxin treatment and antibiotics as soon as possible, reducing the risk of complications and transmission.
Diphtheria is a medical emergency that requires immediate treatment to prevent severe complications and reduce the risk of transmission. Early treatment significantly reduces the risk of complications and death, highlighting the importance of prompt medical intervention. The treatment approach involves neutralising the toxin, eliminating the bacteria and providing supportive care.
The diphtheria toxin is the primary cause of severe complications. To counteract its effects, patients receive a diphtheria antitoxin which neutralises the toxin before it binds to tissues. This treatment is most effective when administered early, as it does not reverse damage already caused by the toxin. Before administering DAT, doctors perform an allergy test to check for sensitivity. (1)
To eliminate Corynebacterium diphtheriae from the body and prevent further spread, doctors prescribe antibiotics such as:
Patients are considered non-infectious after completing a full antibiotic course and testing negative for the bacteria. (1)
Hospitalisation is often necessary, especially in severe cases where patients require:
Since diphtheria spreads easily, infected individuals are isolated to prevent outbreaks. Close contacts, including family members and caregivers may receive antibiotics and booster vaccinations as a precaution.
Having diphtheria does not provide lifelong immunity, so recovered patients must receive a full diphtheria toxoid vaccine series to prevent reinfection. Booster doses are recommended every 10 years.
Preventing diphtheria requires a combination of vaccination, good hygiene and public health interventions to limit transmission. Since the disease spreads through respiratory droplets and direct contact, preventive measures play a crucial role in reducing outbreaks.
Fig. 4: Showing diphtheria prevention plan. Click on image to enlarge.
The diphtheria vaccine is the most reliable and effective way to prevent infection. It is given as part of combination vaccines that protect against multiple diseases (3):
High vaccination coverage in communities creates herd immunity, reducing the risk of outbreaks. Immunity from the diphtheria vaccine wanes over time, making booster doses such as Td or Tdap essential. Unvaccinated individuals should receive a full vaccine series to ensure immunity.
Since diphtheria spreads through respiratory droplets and contaminated surfaces, maintaining good hygiene helps prevent transmission. Some key practices include:
Prompt identification and treatment of diphtheria cases help contain outbreaks. Public health authorities encourage people to seek medical attention if they experience symptoms such as a sore throat, breathing difficulties or a thick membrane in the throat.
During outbreaks, health authorities implement measures such as:
Travellers to regions where diphtheria is common should ensure they are fully vaccinated before departure. Those returning from affected areas should monitor their health and seek medical attention if symptoms appear.
By prioritising vaccination, maintaining hygiene and ensuring rapid medical response, diphtheria can be effectively controlled, thereby reducing the risk of severe illness and death.
Controlling diphtheria requires a coordinated public health response to prevent outbreaks, limit transmission and ensure effective treatment. Governments implement various strategies to contain the disease and protect communities. Here are some of these strategies:
Governments and health organisations need to run routine immunisation programmes to ensure high vaccine coverage. Special vaccination campaigns should be launched in outbreak-prone areas to increase community immunity.
Early detection of diphtheria cases helps in preventing outbreaks. State-of-the-art laboratories should be provided to assist in identification and confirmation of cases through bacterial cultures and toxin tests. Surveillance systems should be put in place to track cases and identify high-risk areas for targeted and prompt intervention.
To prevent the spread of diphtheria, infected individuals are isolated while healthcare workers follow strict infection control measures, such as wearing protective gear and disinfecting surfaces while hospitals enforce airborne and droplet precautions to minimise transmission risk.
Close contacts of infected individuals are identified, monitored for symptoms and, if unvaccinated, given the diphtheria vaccine along with preventive antibiotics like erythromycin or penicillin to reduce the risk of infection.
Health authorities conduct educational campaigns to inform people about diphtheria symptoms, transmission and prevention. This is also an avenue to combat vaccine misinformation with evidence. Schools, workplaces and communities are encouraged to promote hygiene practices such as handwashing and respiratory etiquette.
Hospitals and clinics should be equipped with antitoxins, antibiotics and critical care facilities especially in high-risk areas. Training for healthcare workers also ensures early diagnosis and appropriate treatment.
International health organisations provide guidance to countries facing outbreaks while also advising travellers travelling to endemic areas to be fully vaccinated.
By implementing these control measures, governments and health agencies can minimize the spread of diphtheria, protect vulnerable populations, and prevent large-scale outbreaks.
Diphtheria is a preventable yet persistent threat, particularly in areas with low vaccination rates and weak healthcare systems. While medical advancements have made the disease manageable, outbreaks still occur, showing the need for continuous immunisation efforts and early detection.
Protecting communities from diphtheria requires collective efforts such as, ensuring children receive routine vaccinations, strengthening healthcare infrastructure and countering misinformation that discourages immunisation. Governments and health organisations must also prioritise access to vaccines, improve outbreak response strategies and enhance public awareness.
With sustained commitment to prevention, early diagnosis and timely treatment, diphtheria can be kept under control, reducing its impact and safeguarding future generations from this potentially deadly disease.
1. Lamichhane, A, & Radhakrishnan, S. Diphtheria. StatPearls Publishing. [Internet], (Updated February 26, 2024). Cited March 27, 2025, Available from here
2. New York State Department of Health. Diphtheria fact sheet. Last reviewed Jan.2012. [Cited March 27, 2025]. Available from here
3. Centers for Disease Control and Prevention. Diphtheria: About diphtheria. U.S Department of Health & Human Services. [Internet]. Feb 4, 2024. [Cited March 27, 2025]. Available from here
Related: Diphtheria Cases Rise in Nigeria as Lagos Becomes Worst-hit State
Published: March 30, 2025
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content for non-commercial purposes without alteration or modification and subject to attribution as to source.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.