Gonorrhoea Eye Infection in the Newborn: What Africans Need to Know
By Chinedu Akpa. B. Pharm. Freelance Health Writer, with medical and editorial review by the DLHA Team

A newborn with swollen eyelids, and thick yellow-coloured discharge, likely due to birth-related infection
The eye is often referred to as the body's light, but what happens when a neonate (newborn baby) has gonorrhoea eye infection and this gets in the way, preventing them from ever seeing that light? What if they never get to set their eye on that person who birthed them? As rhetorical as these questions may sound, they describe the struggle that infants have to face as soon as they are delivered if they were to have gonorrhoea eye infection.
Neonatal gonorrhoea eye infection (NGEI) or neonatal gonococcal eye infection is usually transmitted from a mother to her child during birth as the baby passes through the vagina.
How does this happen?
What organism is responsible for this disease?
How can the condition be prevented?
These questions and more will be tackled and answered in this article. So, read on!
Neonatal gonococcal eye (NGEI) infection is a priority eye disease in the newborn. It is estimated to have a 1% worldwide prevalence rate. While the rate is substantially lower in developed nations like in Europe and North America, it is significantly higher in developing nations like in Africa, where the gonococcal infection rate among pregnant women is nearly 5% in some regions. [1]
NGEI occurs when a mother fails to treat gonorrhea infection which is then passed to her baby (vertical transmission) during birth through secretions of the causal organism in the vagina. [2]
If the infection is not treated, the child may experience serious complications like infection of the tissue lining the eyes and inner part of the eyelids (conjunctivitis), wound to the cornea (corneal ulceration), corneal scarring, long-term eye damage, or even blindness.
Neisseria gonorrhoeae is the organism that causes neonatal gonococcal eye infection. This is made possible because the cervix and urethra (the tube that passes urine out of the body) of the mother acts as a storage for the organism. Although the vaginal canal is the primary route of transmission, it is possible for a mother to pass this organism to her child after having a cesarean session. [1] Even with precautionary measures in place, such as prophylaxis with antibiotics, approximately 1 in every 100 neonates exposed to gonorrheal secretion may still develop a neonatal gonococcal eye infection. [1]
In contrast to men, the majority of women do not typically exhibit gonorrhea symptoms. [3] This could help to explain why some of them, particularly in resource-poor continents like Africa, can spread the infection to their offspring without being aware that they are carriers of the infection.
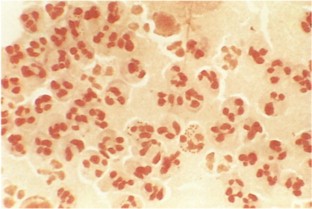
Microscopic appearance of gram-stained sample of eye discharge from a newborn showing characteristics suggestive of Neisseria gonorrhoeae infection (i.e., gram-negative intracellular diplococci).
Neisseria Gonorrhoeae (NG) is a bacterium (germ) that causes gonorrhea, a well-known Sexually Transmitted Infection (STI). It inhabits human cells, including those of the cervix, urethra and vagina in women and resembles a kidney bean under a microscope. It cannot survive outside the human cell for more than 24 hours. [4]
NG has certain properties that allow it to evade the body's immune system's actions, help it stick to human cells, and make it difficult to remove and simple to harm humans. Additionally, the organism produces an agent (beta lactamase) that aids in the breakdown of antibiotic medications, making it possible to develop antibiotics resistance. [4]
While the symptoms of a neonatal gonococcal eye infection can be easily confused with those of other eye infections in newborns, a doctor may be able to diagnose a neonatal gonococcal eye infection in your child if specific symptoms are present. These symptoms include:
When diagnosis and treatment aren't carried out on time, severe complications may occur and these include:
Correct diagnosis of NGEI is crucial because there are several other neonatal eye conditions and infections caused by different agents and germs (organisms) that can be mistaken for it.
Common chemical agent causing newborn eye infections
Common organisms causing newborn eye infections
A thorough physical examination of the baby by the doctor and a review of the parents' medical history are the first steps in the diagnosis process.
Since symptoms can be confusing, timing has emerged as a crucial tool for examining clinical presentation features.
For example, if symptoms such as redness and swelling of the eyelids (erythema), swelling of the conjunctiva, and murky eye discharge appear in the eyes of a newborn baby within 24 hours of delivery, chemical conjunctivitis is usually suspected.
Symptoms of neonatal gonococcal infections usually appear 2–5 days after delivery, whereas Chlamydia trachomatis symptoms appear 5–14 days after birth. [5]
A laboratory test called Gram stain is usually coupled with culture of a murky eye discharge and performed when the germ (organism) causing eye infection in the newborn is suspected to be Neisseria gonorrhoeae. These tests help to correctly identify the causative germ and ensure proper medication is given with better outcomes. [5]
Other advanced tests are used to differentiate eye infections due to Chlamydia trachomatis infection from those due to NG. [5]
Between 30% and 50% of newborns who don't receive preventive treatment (prophylaxis) for neonatal gonococcal eye infections are at risk of developing the condition, which can lead to wounds on the surface of the eyes (corneal ulceration) or permanent vision loss. [6]
The earliest preventive treatment used was silver nitrate eye drops, but it was discontinued due to side effects like chemical conjunctivitis. Alternatives like antibiotic eye drops or ointments such as gentamicin and tetracycline have also been limited due to severe reactions and development of resistance. [6]
The best prevention is screening and treating pregnant women with Neisseria gonorrhoeae infections. However, since not all women are tested, the CDC recommends prophylaxis using erythromycin eye ointment for all newborns. If erythromycin is unavailable, a single dose of ceftriaxone (25–50 mg/kg IV or IM) can be given. [7]
For all babies, whether delivered vaginally or via Caesarean section, 0.5% erythromycin ointment should be applied to both eyes shortly after birth, usually as a one-time treatment. [7]
The U.S. Preventive Services Task Force (USPSTF) advises screening pregnant women at risk of gonorrhoea infection, including those under 25, or over 25 with high-risk factors (e.g., multiple partners, STIs, or living in areas with high gonorrhoea rates). Pregnant women with infections should be retested every three months, in the final trimester, or before delivery. [7]
Neonatal gonococcal eye infections are treated with a combination of topical and systemic antibiotics with other supportive care as follows:
Systemic treatment: This involves the use of a single dose of the antibiotic called ceftriaxone (25–50 mg/kg) given into baby's muscle (IM) or vein (IV). If ceftriaxone is unavailable, cefotaxime (100 mg/kg) can be used. [7]
Topical treatment: Apply erythromycin (antibiotic eye ointment to both eyes every 2 - 4 hours
Supportive treartment: Use sterile salt solution to rinse the eye and rid them of the murky discharge.
Prompt treatment of this condition is vital to prevent complications like wound to the tissue covering the surface of the eyes (corneal ulceration) and blindness. The mother of an infected infant and her sexual partner should also be treated for gonorrhoea infection.
In conclusion, neonatal gonococcal eye infection is a serious condition that can lead to long-term visual impairment or blindness if left untreated. Early detection through screening of pregnant women, along with timely prophylactic measures like erythromycin eye ointment for newborns is essential for prevention. Prompt diagnosis and treatment with appropriate antibiotics can significantly reduce complications, ensuring that affected infants have the best chance for healthy eye development and overall well-being.
References
1. Costumbrado J, Ng DK, Ghassemzadeh S. Gonococcal Conjunctivitis. [Updated 2022 Sep 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from here.
2. Medscape. Neonatal Conjunctivitis (Ophthalmia Neonatorum) Clinical Presentation. [Internet, n.d]. Cited October 2nd, 2024. Available from here.
3. World Health Organisation. Gonorrhoeae (Neisseria gonorrhoeae infection). [Internet, n.d]. Cited October 2nd, 2024. Available from here.
4. Canada Public Health Services Laboratory. Neisseria gonorrhoeae: Infectious substances pathogen safety data sheet. [Internet, n.d] cited October 3, 2024. Available from here.
5. Castro Ochoa KJ, Mendez MD. Ophthalmia Neonatorum. [Updated 2023 Jan 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from here.
6. Moore DL, MacDonald NE; Canadian Paediatric Society, Infectious Diseases and Immunization Committee. Preventing ophthalmia neonatorum. Can J Infect Dis Med Microbiol. 2015 May-Jun;26(3):122-5. doi: 10.1155/2015/720726. PMID: 26236350; PMCID: PMC4507834. Available from here.
7. US Centers for Disease Control (CDC). Gonococcal Infection Among Neonates. [Internet n.d]. Cited October 4, 2024. Available from here.
Published: October 12, 2024
© 2024. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content freely for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.