How the Sickle Cell Trait Protects Against Malaria: A Simplified Scientific Explanation
By: Tii Ngwachi Munghieng, MD. Medically reviewed by A. Odutola; MBBS, PhD, FRCSEd
.jpg)
Did you know that up to 30% of people in sub-Saharan Africa carry the sickle cell trait? This physical trait not only affects health but has helped shape human survival (evolution) in regions where malaria is common.
The relationship between the sickle cell trait (SCT) and malaria is one of the most interesting examples of how human traits that are passed from parents to their children (genetics) adapt to environmental challenges.
Found predominantly in regions like sub-Saharan Africa where malaria is common, SCT offers natural protection against severe malaria caused by Plasmodium falciparum, the deadliest of the malaria parasites carried by the anopheles mosquito.
However, this protective trait comes with trade-offs, as it increases the likelihood of sickle cell disease (SCD) in certain populations.
This article explains the scientific link between SCT and malaria protection, explores its development over generations and its public health implications.
To understand SCT, we need to know a little about hemoglobin, the protein in red blood cells that carries oxygen throughout the body.
In people with normal hemoglobin genes, red blood cells are round and flexible, allowing them to flow freely through blood vessels. But in people with the sickle cell gene (HbS), red blood cells sometimes become stiff and shaped like a crescent (half-moon) or sickle.
.jpg)
Fig. 1: Showing inheritance pattern of the sickle cell trait and disease
When you inherit one normal hemoglobin gene (HbA) and one sickle cell gene (HbS) from your respective parents you will carry the Sickle Cell Trait (HbAS) (see fig. 1). This does not cause health problems in most cases.
When you inherit two sickle cell genes (HbS). from your parents, you will have Sickle Cell Disease (HbSS) (see fig. 1). This condition leads to severe complications such as anemia, pain crises, and organ damage.
People with SCT (HbAS) have a unique advantage. They are better protected against malaria compared to those with normal hemoglobin (HbAA) or sickle cell disease (HbSS).
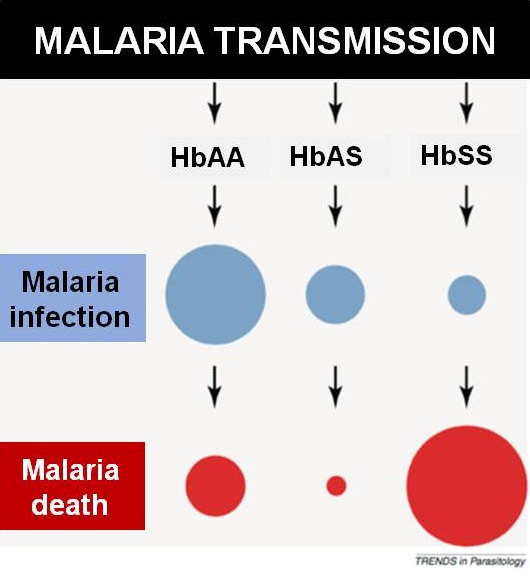
Illustration showing how the sickle cell trait protects against malaria transmission. Click on image to enlarge. Image credit: Williams TN, Obaro SK, 2011.
Malaria is caused by parasites called Plasmodium species with the most severe form being Plasmodium falciparum that invades red blood cells. In people with SCT, several mechanisms make it difficult for the parasite to survive:
The sickle-shaped red blood cells in SCT carriers are less hospitable to malaria parasites. When the parasite enters these cells, it struggles to grow and multiply because the environment is not ideal. [1]
In SCT carriers, the sickled cells that contain parasites are quickly detected and destroyed by the immune system. This prevents the parasite from spreading further. [2]
Malaria parasites need oxygen to survive, but sickled red blood cells cells have lower oxygen levels. This creates an unfriendly environment for malaria parasites to survive and gives people with SCT a natural protection against severe malaria. [3]
The connection between sickle cell disease (SCT) and malaria protection was first observed in 1954 by Anthony Allison. He discovered that individuals with SCT in East Africa were far less likely to die from malaria than those without the trait. [1]
Further studies have confirmed this protective effect:
These studies show how natural selection has played a critical role in maintaining the sickle cell gene in areas where malaria is common.
The widespread presence of SCT in malaria-prone regions is a clear example of balancing selection, where a genetic trait persists because it offers both benefits and risks.
3. Trade-Offs
While SCT protects against malaria, it increases the likelihood of SCD when two carriers reproduce. This shows the evolutionary compromise: the benefit of surviving malaria outweighs the risk of producing children with SCD at the population level. [7]
The relationship between SCT and malaria presents both opportunities and challenges for public health. These include;
SCD is a significant health burden in regions with high SCT prevalence. Without proper care, it can lead to severe complications and early death. Solutions include:
By reducing malaria transmission, the burden of SCT may also be reduced. Key strategies include;
Public health campaigns can help communities understand the benefits and risks of SCT. This will help them to make informed decisions about health and reproduction.
Kenya, a country in East Africa, shows the dual impact of SCT and malaria:
Kenya has responded by:
Advances in science and medicine offer hope in addressing the challenges posed by Sickle Cell Trait and malaria. Some of the possible solutions include;
1. Gene editing
Technologies like CRISPR could potentially “fix” the sickle cell gene, and cure SCD while preserving malaria resistance. [9]
Advances in science and medicine offer hope in addressing the problems created by SCT and malaria.
The combination of efforts between researchers, healthcare providers, and governments can ensure better outcomes for individuals affected by both malaria and SCD.
The sickle cell trait is a good example of how human traits and behaviours that pass through generation (i.e., genetics), adapt to environmental challenges. Its ability to protect against malaria has saved countless lives, but it also comes with the risk of sickle cell disease.
Understanding the sickle cell trait's role in protecting against malaria could transform global health efforts to fight both conditions. Genetic counseling and malaria prevention programs remain critical in reducing malaria and sickle cell disease burden in Africa.
By combining malaria control programs with genetic counseling and advanced treatments for SCD, the health and well-being of millions of people in Africa and worldwide can be improved consierably.
1. ALLISON AC. Protection afforded by sickle-cell trait against subtertian malarial infection. Br Med J. 1954 Feb 6;1(4857):290-4. doi: 10.1136/bmj.1.4857.290. Available from here.
2. Williams TN, Mwangi TW, Wambua S, Alexander ND, Kortok M, Snow RW, Marsh K. Sickle cell trait and the risk of Plasmodium falciparum malaria and other childhood diseases. J Infect Dis. 2005 Jul 1;192(1):178-86. doi: 10.1086/430744. Available from here.
3. Taylor SM, Parobek CM, Fairhurst RM. Haemoglobinopathies and the clinical epidemiology of malaria: a systematic review and meta-analysis. Lancet Infect Dis. 2012 Jun;12(6):457-68. doi: 10.1016/S1473-3099(12)70055-5. Available from here.
4. Aidoo M, Terlouw DJ, Kolczak MS, McElroy PD, ter Kuile FO, Kariuki S, Nahlen BL, Lal AA, Udhayakumar V. Protective effects of the sickle cell gene against malaria morbidity and mortality. Lancet. 2002 Apr 13;359(9314):1311-2. doi: 10.1016/S0140-6736(02)08273-9. Available from here.
5. Weatherall DJ, Clegg JB. Inherited haemoglobin disorders: an increasing global health problem. Bull World Health Organ. 2001;79(8):704-12. Available from here.
6. Carter R, Mendis KN. Evolutionary and historical aspects of the burden of malaria. Clin Microbiol Rev. 2002 Oct;15(4):564-94. doi: 10.1128/CMR.15.4.564-594.2002. Erratum in: Clin Microbiol Rev. 2003 Jan;16(1):173. Available from here.
7. Hedrick, P. Population genetics of malaria resistance in humans. Heredity 2011; 107, 283–304 (2011). https://doi.org/10.1038/hdy.2011.16. Available from here.
8. Luzzatto L. Sickle cell anaemia and malaria. Mediterr J Hematol Infect Dis. 2012;4(1):e2012065. doi: 10.4084/MJHID.2012.065. Available from here.
9. Singh A, Irfan H, Fatima E, Nazir Z, Verma A, Akilimali A. Revolutionary breakthrough: FDA approves CASGEVY, the first CRISPR/Cas9 gene therapy for sickle cell disease. Ann Med Surg (Lond). 2024 May 15;86(8):4555-4559. doi: 10.1097/MS9.0000000000002146. Available from here
Related:
Published: February 13, 2025
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.