Lewy Body Dementia: What Africans Need to Know
By Oluwasola Samuel, freelance health writer. Medically reviewed by A. Odutola, MBBS, Ph.D., FRCSEd.
An elderly Afriacn man looking pensive with his left hand on his cheek
When there is a discussion about dementia, people often think of Alzheimer's disease. But other types of dementia less talked about include Lewy Body Dementia (LBD).
This condition, though less well-known, is the next most common form of irreversible dementia associated with the degeneration of brain cells, after Alzheimer's disease. [1] Yet, in Africa, many people have never heard of it. A lack of awareness can lead to delays in diagnosis and treatment.
In this article, you will learn about Lewy Body dementia from these viewpoints:
Lewy body dementia (LBD) is a brain condition that affects how people think, move, and feel. It is one of the most common types of dementia after Alzheimer’s disease, but many people don’t know about it.
Lewy body dementia occurs due to the deposits of abnormal substances (proteins) called alpha-synuclein in the brain cells. These abnormal proteins build up and damage the nerve cells of the brain.
Once damaged, the brain cells stop working properly. The parts of the brain responsible for thinking, memory, movement, and even mood are most affected.
How Common is Lewy Body Dementia in sub-Saharan Africa?
Lewy body demetia (LBD) remains largely underreported in sub-Saharan Africa, but its presence is real and growing as the region's elderly population rises.
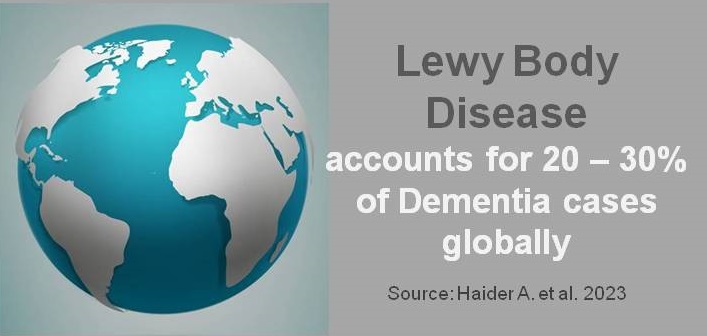
Relative burden of Lewy body dementia among dementia cases globslly. Source.
Studies have shown that dementia in general, is becoming more common in Africa. [2] This is happening as a result of ageing, lifestyle changes, and increasing rates of diseases like high blood pressure and diabetes, which are risk factors for LBD.
Globally, LBD accounts for about 20%–30% of all dementia cases, but data specific to Africa is sparse because of limited research and diagnostic challenges.
According to estimates, over 2 million people in sub-Saharan Africa were living with dementia as of 2015, and this number is expected to double every 20 years due to population growth and longer life expectancy. [3]
While exact figures for LBD are unclear, studies in similar low- and middle-income countries suggest that it could make up a significant portion of dementia cases. This means hundreds of thousands of Africans may already be living with LBD, often without proper diagnosis or support.
There are two main types of Lewy body dementia (LBD), and while they have many similarities, they also have unique differences.
Let’s break them down so you can understand:
This type of LBD largely affects nerve cells in parts of your brain (cerebral cortex) that control how you think and remember things (see fig. 1). If you are living with dementia with Lewy bodies (DLB), you may first experience confusion, difficulty focusing, or trouble understanding things. You also have hallucinations (seeing or hearing things that aren’t there). For example, a person with this condition might say they see children playing in their living room, even when there’s no one around.
Over time, you may also have problems with movement. Your body might feel stiff, your hands might shake, or you might begin to walk slower than before, just like someone with Parkinson’s disease.
Illustration showing types of Lewy Body Dementa with areas of the brain commonly affected. Click on image to enlarge.
This type of Lewy body dementia starts differently. It affects nerve cells located in parts of your brain that control movement, called the cerebellum, and brainstem (see fig. 1). It also occurs in people who already have Parkinson’s disease, a movement disorder. People with Parkinson’s disease usually have symptoms like shaking hands, stiff muscles, or trouble balancing.
If you are living with Parkinson's disease and you develop memory loss and confusion one year or more after you begin to experience movement problems, it's called Parkinson’s disease dementia.
The difference between dementia with Lewy body (DLB) and Parkinson's disease dementia (PDD) is the timing of symptoms. In DLB, memory and thinking problems happen first, and movement issues appear later. In PDD, movement issues like shaking and stiffness happen first, and thinking problems come later.
Knowing the difference will help caregivers and family members who have people living with either of the conditions identify the condition earlier.
Lewy Body Dementia (LBD) progresses in stages over time, just like many other types of dementia. These stages can vary from person to person. There are three phases of Lewy body dementia.
These stages include:
Early stage
In the early stage, you may experience mild symptoms. Sometimes, you may not even realise something is wrong.
At the early stage, you may experience the following:
Middle stage
As Lewy body dementia progresses, the symptoms become more noticeable and may start affecting your daily life. This means you will need a caregiver to help you with your personal care and daily activities.
At the middle stage, you may experience the following:
Late-stage
In the late stage, the symptoms are serious, and the person needs help with almost everything (self-care and daily activities).
At the late stage, you may experience the following:
Not everyone with LBD experiences similar symptoms. The severity of symptoms can vary.
A person with Lewy body dementia may not have every symptom.
The common symptoms of LBD include the following:
Some of the symptoms may be mistaken for normal ageing or even spiritual attacks.
What Causes Lewy Body Dementia?
The cause of Lewy body dementia is still unknown, but it is often associated with deposits of an abnormal protein called alpha-synuclein (Lewy body) in cells of the brain. The alpha-synuclein distorts the function of the part of the brain responsible for thinking, memory, mood, and movement.
Researchers have identified several risk factors for the condition [5]
Some risk factors of Lewy body dementia that have been identified include:
1. Age
People who are over 50 years old are at a bigger risk of having Lewy body dementia. [6] The risk of Lewy body dementia increases as you age.
If you have a history of Lewy body dementia in your family, you are at risk of having it later on in life. This means that if someone like your parent or sibling had dementia or Parkinson’s disease, your risk might be higher.
3. Sex
Sex is also a risk factor when it comes to Lewy body dementia. Research suggests men are at higher risk of having Lewy body dementia compared to women. [7]
Some health conditions may increase your risk of having Lewy body dementia. Conditions like REM (sleeping behaviour disorder), Parkinson's disease, high blood pressure, high cholesterol, and diabetes.
It’s important to note that having one or more of these risk factors doesn’t mean you’ll have Lewy body dementia—it just means your chances of having the condition are higher.
The diagnosis of LBD begins with a detailed history and examination by your healthcare provider, preferably someone with special training in neurology—a field of medicine that focuses on the disorders that derail the normal functions of the brain, spinal cord, and nerves.
During history taking, your healthcare provider will listen to your complaints and ask several questions including:
Following the history-taking, your healthcare provider will perform a full general and neurological examination and may order some tests.
Note that no single test can diagnose Lewy body dementia with 100% accuracy. There is a need for several tests or evaluations to be carried out to exclude other conditions and confirm a diagnosis.
The tests that are conducted may include:
A mental examination checks the level of your memory and thinking capabilities, including:.
Blood tests may be carried out as part of a general health check as well as to help rule out other health conditions that can affect brain function, like thyroid and liver problems, HIV or vitamin B-12 deficiency.
This test involves puncturing the lower part of the spinal cord with a needle-like device. Once punctured, the needle-like device is used to collect fluid that originates from and bathes the brain and the spinal cord (cerebrospinal fluid). The fluid is then checked for the level of the abnormal protein (alpha synuclein) associated with Lewy body dementia. While this test shows promise in the diagnosis of LBD, it is currently not used as a routine diagnostic test.
Brain scans such as magnetic resonance imaging (MRI) and computed tomography scans (CT) are imaging scans that give a clear and detailed image of the brain. The images help your healthcare professional to check for abnormalities of structure in the brain.
Other imaging tests that can be carried out to check for functional abnormalities, include:
After the clinical evaluation and tests are carried out, your healthcare professional would be in a better position to make an informed working diagnosis of your condition and discuss a treatment plan with you.
Note that a definitive diagnosis of Lewy Body Dementia can only be made after death when the brain is studied in the laboratory.
The diagnosis of LBD and other dementia disorders in Africa comes with unique challenges that may make it difficult for you to get the right diagnosis and treatment.
Some of these challenges include:
Many areas (rural areas) in Africa don’t have enough hospitals or clinics. People may have to travel long distances to see a doctor, which can delay or prevent diagnosis and treatment. For example, a person living with Lewy body dementia or other health conditions may be discouraged from embarking on a long journey just to get diagnosed. The person might prefer to seek quick and alternative solutions.
2. Lack of Specialists
Diseases like Lewy body dementia require high level medical specialists (neurologists, psychiatrists, geriatricians, and others), but there are very few of them in many African countries. This leaves a gap in the number of specialists needed to cater for complex conditions like Lewy body dementia and other related conditions. [8]
Many people, including healthcare workers, may not know much about Lewy body dementia. They might think the symptoms are those of normal ageing, stress, or even spiritual issues instead of recognising it as a medical condition. Due to low awareness, this condition is misdiagnosed or ignored.
4. Cultural Beliefs and Stigma
Some communities in Africa may view memory loss or behavioural changes as witchcraft, punishment, or a normal part of ageing, instead of seeking medical help. Fear of being judged can prevent a person from visiting the hospital.
Advanced tests like brain scans (MRI, PET, or CT scans) are expensive and not affordable for many people. Even basic tests may cost more than some families can afford due to low purchasing power. As a result, many families might prefer to see other alternative means of diagnosis or treatment.
Many hospitals in Africa don’t have the equipment needed to check for dementia or other brain disorders. Without tools like brain scans or specific blood tests, doctors can only make conclusions based on symptoms and physical examination findings. This could increase the chances of inaccurate diagnosis being made.
7. Overburdened Healthcare Systems
Doctors and nurses in many parts of Africa are overworked because there aren’t enough healthcare workers for the population served. [8] With so many patients to see, they might not have the time to evaluate and treat people with complex symptoms like those of dementia properly.
To overcome these challenges, the government and other stakeholders need to:
Lewy body dementia is a challenging condition to treat. The sad truth is that this condition has no cure. However, treatment and management methods can help improve symptoms and quality of life.
Treatment and management options include:
Doctors may prescribe medications to manage the different symptoms of LBD.
Here are the main ones:
Cholinesterase inhibitors such as rivastigmine, memantine, or donepezil can be administered to improve memory, alertness, and thinking.
Levodopa may help improve movement problems similar to Parkinson’s, but it can sometimes worsen hallucinations.
Your healthcare professional may use very low doses of antipsychotic medications like quetiapine. However, many antipsychotic medications can worsen LBD symptoms. As a result, it must be used with caution.
Melatonin or certain sleep medications like Clonazepam might help improve sleep quality.
For feelings of depression and anxiety, antidepressants can help manage feelings of sadness or worry.
Non-drug therapies are essential for improving daily life and overall well-being. They require no drugs.
Some of these therapies include:
Physical therapy improves your strength and balance and reduces the risk of falling over time. A physiotherapist will select the best exercises that improve strength and flexibility.
An occupational therapist teaches ways to manage daily tasks more easily, like eating, dressing, or bathing. Occupational therapy promotes functional ability and independence.
This therapy helps with speech and swallowing problems, which may occur as LBD progresses. A speech-language specialist assists in improving your ability to swallow, talk, and express your thoughts.
A neuropsychologist helps carry out cognitive training. This form of therapy involves activities that keep your brain engaged. Activities include memory games, puzzles, or problem-solving exercises.
Making small changes at home can help manage LBD symptoms. These include:
You can join a support group for patients or caregivers that provide emotional and practical help. You can also talk to a therapist to help manage stress, anxiety, or depression.
As Lewy body dementia affects memory, movement, and mood, caregivers need to learn how to handle different symptoms.
For example, if a patient hallucinates, calmly reassure them rather than argue with them.
Caregivers should also take care of themselves to avoid burnout, which might lead to reduced quality of care.
Some drugs, like strong antipsychotics, anticholinergics, or antidepressants, can make LBD symptoms much worse. It’s important to talk to doctors before starting any new medicine.
While there’s no guaranteed way to prevent Lewy body dementia (LBD), you can take steps to help lower your risk or delay its onset. Factors like genetics and ageing are beyond our control, so prevention is nearly impossible. [9] However, a healthy lifestyle is key—regular exercise, a balanced diet rich in fruits, vegetables, and healthy fats (leafy greens, beans, and fish), and engaging in brain-tasking activities like puzzles, learning, or storytelling.
Managing chronic conditions like high blood pressure and diabetes is also crucial, as these can increase dementia risk. Access to nutrient-rich foods gives Africa a head start.
How long someone lives with Lewy body dementia (LBD) can vary a lot from person to person. On average, people with LBD live about 5 to 8 years after symptoms start, but some may live longer—up to 20 years in rare cases. [5] It depends on factors like their overall health, the age when symptoms begin, and how quickly the disease progresses.
The key thing is to focus on quality of life. With the right care—like managing symptoms, staying physically active, and having a strong support system—someone with LBD can still enjoy meaningful moments with loved ones.
LBD is a progressive disease, meaning symptoms develop gradually and worsen over time. Lewy body dementia (LBD) typically begins between the ages of 50 and 85, with the majority of cases diagnosed in individuals over the age of 50. It is relatively rare for LBD to occur in people younger than 50.
Caring for someone with Lewy body dementia (LBD) involves creating a calm, safe environment and sticking to a consistent routine to ease confusion and agitation. Be patient and use simple words to communicate. Watch for symptom changes like hallucinations or mobility issues and consult with a healthcare provider as needed.
Encourage light physical activity and engaging, low-stress mental activities.
Prioritise a healthy diet, hydration, and addressing sleep problems. Offer plenty of emotional support, as LBD can be scary and frustrating for them. Don’t forget to take care of yourself too—seek support to stay strong for your loved one.
Lewy body dementia (LBD) can lead to death, as it is a progressive disease that worsens over time. While LBD itself doesn’t directly cause death, complications like severe mobility issues, swallowing difficulties, infections (e.g., pneumonia), or falls can become life-threatening.
You should see a doctor if you or a loved one notice persistent or worsening symptoms like memory loss, confusion, visual hallucinations, movement issues (stiffness or tremors), or sudden changes in alertness or behaviour. These could be signs of Lewy body dementia or another condition that needs attention. Early diagnosis helps manage symptoms better, so don’t hesitate to reach out if something feels off.
Lewy body dementia (LBD) is a progressive brain disorder that impacts thinking, movement, and behaviour, yet it remains poorly understood in Africa. Symptoms like cognitive fluctuations, visual hallucinations, and Parkinson's-like movement issues are often overlooked or misdiagnosed, leaving families struggling to cope.
Low awareness and cultural stigma around dementia further delay diagnosis and access to care, creating challenges for patients and caregivers alike. However, change is possible. There is a need for constant awareness to break the stigma and ensure better support for those affected.
1. Prasad S, Katta MR, Abhishek S, Sridhar R, Valisekka SS, Hameed M, et al. Recent advances in Lewy body dementia: A comprehensive review. Disease-a-Month 2023 May 1 69(5):101441. Doi: 10.1016/j.disamonth.2022.101441. Available from here.
2. Haider A, Spurling BC, Sánchez-Manso JC. Lewy body dementia. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Last updated Feb. 12, 2023. [Cited 2025 Mar 1]. Available from here.
3. Kehoua G, Dubreuil CM, Ndamba-Bandzouzi B, Guerchet M, Mbelesso P, Dartigues JF, et al. People with dementia in sub-Saharan Africa: Results of the Epidemca-Fu program in the Congo. Dement Geriatr Cogn Dis Extra 2019 Apr 3;9(1):163–75. Available from here.
4. Alzheimers. Gov. What is Lewy body dementia? | [Internet]. Last updated: Sept 18, 2024. [Cited 2025 Mar 1]. Available from here.
5. National Institute of Neurological Disorders and Stroke. Lewy body dementia | [Internet, n.d.]. [Cited 2025 Mar 1]. Available from here.
6. National Institute on Ageing. Lewy body dementia: causes, symptoms, and diagnosis. [Internet]. Last reviewed Jan. 27, 2025. [Cited 2025 Mar 1]. Available here.
7. Lewy Body Dementia Association. Men are at greater risk for Lewy body dementia than women, but why? A new study seeks answers. [Internet]. Dec. 12, 2023. [Cited 2025 Mar 1]. Available from here.
8. Olufemi A., ‘There won’t be enough people left’: Africa struggles to stop the brain drain of doctors and nurses. The Guardian [Internet]. 2023 Aug 14. [Cited 2025 Mar 1]. Available from here.
9. National Institutes of Health (NIH). Genetic study of Lewy body dementia supports ties to Alzheimer’s and Parkinson’s diseases. [Internet]. Feb. 16, 2021. [Cited 2025 Mar 1]. Available from here.
Watch the video below to learn more about Lewy Body Dementia
Related
Published: March 18, 2025.
© 2025. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content for non-commercial purposes without alterations or modification and subject to source attribution
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.