Chronic Kidney Disease in Africans: Causes and Symptoms | Chronic Kidney Disease in Africans: Diagnosis and Prevention
By Chinedu Akpa. B. Pharm. Freelance Health Writer, with medical and editorial review by the DLHA Team
Understanding the numerous underlying causes of chronic kidney disease (CKD) has aided in the development of improved management strategies and results.
The approaches to the management of CKD fall under two broad categories:
The non-medication approach to managing CKD involves engaging in healthy living through making adjustment to your lifestyle, thereby reducing your risks of the underlying causes of CKD like hypertension, diabetes, obesity, etc.
When non-medication approach is considered insufficient or inadequate, your doctor would advise you to take medications to manage the underlying causes of your chronic kidney disease (CKD). Ultimately though, dialysis or kidney transplant may be the last resort when CKD progresses to its end stage despite the use of medications to control its underlying causes.
There are different drugs or combination of drugs that are in used to manage different risk factors of CKD. There is no one drug that is specifically used to treat the condition.
You should talk with your doctor to know which medications are best for your condition. The medication information below are brief overviews for informational purposes only. They do not replace the role of your healthcare providers in your care.
High blood pressure is both a cause and an effect of CKD, therefore maintaining a blood pressure of between 130-140/80-90mmHg should be the goal for those with CKD. [12]
Getting your hypertension under control involves making lifestyle changes as well as taking medications. Often, making lifestyle changes alone may be sufficient to keep your blood pressure in check.
 When you need to take medications, the two types of drugs that are usually selected as first-line medications are:
When you need to take medications, the two types of drugs that are usually selected as first-line medications are:
(Examples: Losartan, Candesartan, and Valsartan), and
(Examples: Ramipril, Lisinopril, and Perindopril, etc.
These medications not only help to lower your blood pressure, they also protect the kidney and cardiovascular system from further damage caused by chronic kidney disease (CKD) [13]
Learn more about hypertension and its management of hypertension from here
In addition to making dietary changes and exercise, a group of oral antidiabetics called Sodium-Glucose Cotransporter-2 (SGLT-2) inhibitors of which dapagliflozin is an example, has been found to have multiple functions in controlling some risk factors of CKD, like; controlling the blood sugar and blood pressure as well as helping with weight loss.
SGLT-2 inhibitors drugs are the first choice for people with diabetes and chronic kidney disease (CKD) because they can also enhance kidney function by lowering the amount of protein excreted in the urine. [14]
SGLT-2 inhibitors work to control blood sugar by:
High cholesterol level can be controlled using statins like atorvastatin, and simvastatin in addition to making dietary changes.
The tell-tale indicators of water retention in the body in chronic kidney disease are swollen legs, ankles, face and weight gain.
Water retention is caused by the inability of your kidneys to remove fluid from your body in appropriate amount. To manage this condition, your doctor may recommend that you cut back on fluid and salt intake. If this fails to control water retention sufficiently, your doctor may ask you to take water medications (called diuretics). Some examples of diuretics in common use in Africa, include; thiazides (e.g., Chlorothiazide) and loop diuretics (e.g., Furosemide) recommended.
The glomerulus, is a tiny structures and a part of the kidney nephron. It can become inflamed and lead to kidney disease. Occasionally, this may be brought on by the immune system unintentionally targeting its own cells. Immune system suppressing medications, such as cyclophosphamide or steroids are used to treat this condition.
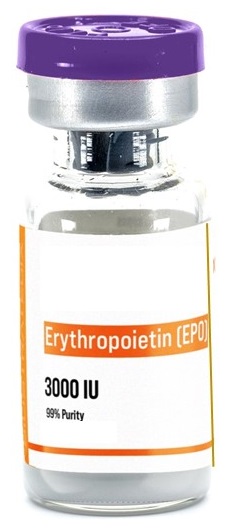 Anemia is a common symptom in many individuals with advanced stages of CKD. The management of anemia in CKD may be complex and involves the use of blood boosting agents, like iron supplements given orally, or by injection or through the blood. It also involves the administration of packed red blood cells transfusion (usually in urgent situations) and the injection of a medication called erythropoietin. This is a hormone produced by the kidney that normally helps to boost red cells production in your bone marrow. The hormone is not produced in sufficient amount in people with CKD. When injected into you however, erythropoietin will stimulate the production of red blood cells in your body, thereby correcting the anaemia associated with CKD.
Anemia is a common symptom in many individuals with advanced stages of CKD. The management of anemia in CKD may be complex and involves the use of blood boosting agents, like iron supplements given orally, or by injection or through the blood. It also involves the administration of packed red blood cells transfusion (usually in urgent situations) and the injection of a medication called erythropoietin. This is a hormone produced by the kidney that normally helps to boost red cells production in your bone marrow. The hormone is not produced in sufficient amount in people with CKD. When injected into you however, erythropoietin will stimulate the production of red blood cells in your body, thereby correcting the anaemia associated with CKD.
Dialysis is the process of drawing waste products out of your body at home or in a medical facility. A small percentage of patients with chronic kidney disease (CKD) would need this procedure for the remainder of their lives. This is typically necessary for those whose kidneys have completely failed.
There are two types of dialysis: [12]
Illustration of a patient hooked up to a haemodialysis machine. Image credit: Nephroplus
Haemodialysis consists of diverting blood from the body to an external machine, where it is filtered before being returned into the body. This is usually done 3 to 4 times every week.
Advantages of haemodialysis include:
Disadvantages of haemodialysis include:
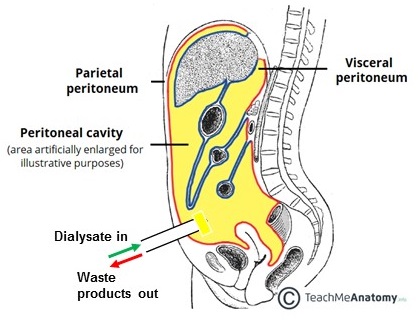
Illustration of peritoneal dialysis setup. Adapted from TeachMeAnatomy.
The peritoneum cavity is a space within your abdomen that contains the following organs: stomach, intestine and liver. It is confined within thin membranes that line the inner surface of your abdominal wall and the outer lining of these organs.
Peritoneal dialysis is the process of introducing a special solution known as the dialysate into the peritoneal cavity. When left for a period, waste products, toxins, excess fluids and salts from the blood that supply the organs of the cavity are filtered or leak into the dialysate and the dialysate is eventually drained out of the body. This process in effect cleanses your blood.
Advantages of peritoneal dialysis include:
Disadvantages of peritoneal dialysis include:
The Kidney Disease Improving Global Outcomes (KDIGO) states that a patient should be referred to a nephrologist if their estimated glomerular filtration rate (eGFR) is less than 30 ml/min/1.73 m², their albumin to creatinine ratio (ACR) is less than 300 mg per 24 hours, or their urine contains more albumin than 2200 mg per 24 hours. [16] This would assist the nephrologist in assessing the need for a kidney transplant (surgery) and replacement therapy.
For people whose kidneys are seriously damaged or no longer function, it is an alternative to dialysis. You may have to wait a long period for this surgery to be performed due to the shortage of donors and donated kidneys. In order for your body to accept the donated kidney, you must also be prescribed immune suppressing drugs for the remainder of your life.
Certain individuals hold the belief that a kidney transplant involving a blood relative must always be successful. However, nephrologist Dr. Abiodun Adeyemo clarified that this is not always the case, adding that a kidney transplant can fail even if the donor is related to you. He went on to say that patients who receive kidney transplants fare better than those who continue on dialysis because kidney transplant recipients have higher survival and better quality of life.
Dr Adeyemo added that the majority of kidney transplants last 10 to 15 years. This is due to the fact that the kidney weakens over time for a variety of reasons, including medication side effects, frequent acute kidney injury, recurrence of the initial disease, and donor and recipient compatibility problems. The majority of transplant-related deaths, he continued, result from complications related to cardiovascular diseases.
In response to a question concerning the prospect of receiving a second transplant, he stated that individuals with chronic kidney disease (CKD) who live long enough can receive a second transplant.
According to Dr. Adeyemo, kidney donation is perfectly safe for the donor and in fact people are encouraged to donate. He said further that although there are risks to the donor, they are related to the surgery rather than the fact that you are left with only one kidney. One kidney can sustain life just as long as two, according to him.
Chronic kidney disease isn’t something that can be fixed with a single magic pill. The kidneys are closely connected to other systems in your body, like your heart, which can make managing CKD more complicated.
Thankfully, better treatments, like the recently discovered SGLT-2 drug group, are giving people with CKD a better chance at living longer. These medications have multiple benefits, making them more effective than traditional options. But medications alone aren’t enough. Incorporating lifestyle changes, like quitting smoking, is just as important in improving treatment oucomes and preventing complications in the long run.
1. Pan American Health Organization. Chronic Kidney Disease. [internet,n.d] cited September 20th, 2024. Available from here.
2. Naicker S. End-stage renal disease in sub-Saharan Africa. Ethn Dis. 2009 Spring;19(1 Suppl 1):S1-13-5. PMID: 19484867. Available from here.
3. Hariparshad S, Bhimma R, Nandlal L, Jembere E, Naicker S, Assounga A. The prevalence of chronic kidney disease in South Africa - limitations of studies comparing prevalence with sub-Saharan Africa, Africa, and globally. BMC Nephrol. 2023 Mar 21;24(1):62. doi: 10.1186/s12882-023-03109-1. PMID: 36944928; PMCID: PMC10029276. Available from here.
4. Vaidya SR, Aeddula NR. Chronic Kidney Disease. [Updated 2024 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: here.
5. National Health Service. Acute Kidney Injury. [internet,n.d] cited September 20th, 2024. Available from here.
6. Wilson S, Mone P, Jankauskas SS, Gambardella J, Santulli G. Chronic kidney disease: Definition, updated epidemiology, staging, and mechanisms of increased cardiovascular risk. J Clin Hypertens (Greenwich). 2021 Apr;23(4):831-834. doi: 10.1111/jch.14186. Epub 2021 Jan 17. PMID: 33455061; PMCID: PMC8035205. Available from here.
7. Vaidya SR, Aeddula NR. Chronic Kidney Disease. [Updated 2024 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from here.
8. Chen TK, Knicely DH, Grams ME. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA. 2019 Oct 1;322(13):1294-1304. doi: 10.1001/jama.2019.14745. PMID: 31573641; PMCID: PMC7015670. Available from here.
9. Center for Disease Control. Testing for Chronic Kidney Disease.[internet,n.d] cited September 20th, 2024. Available from here.
10. Bello AK, Alrukhaimi M, Ashuntantang GE, Basnet S, Rotter RC, Douthat WG, Kazancioglu R, Köttgen A, Nangaku M, Powe NR, White SL, Wheeler DC, Moe O. Complications of chronic kidney disease: current state, knowledge gaps, and strategy for action. Kidney Int Suppl (2011). 2017 Oct;7(2):122-129. doi: 10.1016/j.kisu.2017.07.007. Epub 2017 Sep 20. PMID: 30675426; PMCID: PMC6341007. Available from here.
11. National Kidney Foundation. 7 Golden Rules of Kidney Disease Prevention. [internet,n.d]. Cited September 21st, 2024. Available from here.
12. National Health Service. Treatment; Chronic Kidney Disease. [internet, n.d]. Cited September 21st, 2024. Available from here.
13. Pugh D, Gallacher PJ, Dhaun N. Management of Hypertension in Chronic Kidney Disease. Drugs . 2019 Mar;79(4):365-379. doi: 10.1007/s40265-019-1064-1. Erratum in: Drugs. 2020 Sep;80(13):1381. doi: 10.1007/s40265-020-01388-8. PMID: 30758803; PMCID: PMC6422950. Available from here.
14. Jin ZJ, Wang GZ. Clinical Efficacy of Dapagliflozin in the Treatment of Patients with Diabetic Nephropathy and Its Effect on Proteinuria Level. Diabetes Metab Syndr Obes. 2023 Jul 22;16:2167-2175. doi: 10.2147/DMSO.S421579. PMID: 37502285; PMCID: PMC10370422. Available from here.
15. National Health Service. Pros and Cons of Dialysis. [internet,n.d]. Cited September 23rd, 2024. Available from here.
16. Chen TK, Knicely DH, Grams ME. Chronic Kidney Disease Diagnosis and Management: A Review. JAMA. 2019 Oct 1;322(13):1294-1304. doi: 10.1001/jama.2019.14745. PMID: 31573641; PMCID: PMC7015670. Available from here.
← Chronic Kidney Disease in Africans: Diagnosis and Prevention
Related:
The Kidney: What Every African Needs to Know
Published: September 30, 2024
© 2024. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content freely for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.