By Chinedu Akpa. B. Pharm. Freelance Health Writer and DLHA Volunteer. Medical review and editorial support provided by The DLHA Team

A black pregnant woman in a yellow dress sitting on a couch, holding her lower back with her left hand in apparent discomfort.
A child's cry at birth for those who have been barren for years may be filled with overwhelming joy, relief, gratitude, and a sense of fulfillment. It is also seen as hope for a successor to a throne, continuity of a lineage, or a symbol of pride by many African parents, but this hope is sometimes dashed by obstructed labour, leaving expectant parents heartbroken.
Many women who have stillbirth on the continent blame it on extraterrestrial powers or failure to adhere to certain cultures and traditions. The purpose of this article is to highlight the possible causes of obstructed labour and present possible solutions.
Every year, over 300,000 women die as a result of pregnancy and childbirth complications around the world. [1] According to a 2015 study, obstetric causes contribute approximately 86% of the global burden of maternal deaths, with obstructed labour being one of the direct causes.[1]
A 2019 study of 318 women who gave birth in a general hospital in Ethiopia (Mojo town) found that the prevalence of obstructed labour was 51%, with mis-position (malpresentation), misalignment (malposition), and too large a baby (cephalo-pelvic disproportion) reported as the causes. [2]
During pregnancy, the mother is usually advised not to take or consume anything that will harm the baby, but we often forget that a woman may appear healthy and the baby intact, but delivering the baby, which is dependent on a variety of factors, may hit a brick wall. So, what could go wrong? Obstructed labour! It may not be a term familiar to many, but it is one that some mothers, particularly in Africa, have encountered in some form. So, just what is obstructed labour?
Obstructed labour, as defined by the World Health Organization, means that, despite strong contractions of the womb (uterus), the unborn baby (foetus) cannot pass through the birth canal of the pelvis because there is an unbeatable barrier preventing its movement. The obstruction can occur anywhere along the birth canal, but it usually occurs at its beginning. [3]
Cynthia Ukah, a registered nurse and midwife at Poly General Hospital in Asata, Enugu state, defines it as any labour in which all three components are contributory: a narrow pelvis, a large baby, and an inefficient pelvis.
She further explained that there is a common misconception about obstructed labour in which people believe that women with a large hip will always have a small pelvis (the shape of the pelvis is an important part of childbirth), but this is not always the case, as she clarified in our interview. It is possible to have a large hip and also a big pelvis and vice versa. Pelvic dimensions are more important for childbirth than hip external size, she explained.
Both males and females have pelvises, but the female pelvis differ from male pelvis. Even among women, there are various pelvis shapes. Generally though, the differences in breadth and depth attests to the idea that the female pelvis is fashioned to provide adequate passage for the baby during birth. [4]
There are four types of pelvis, namely: gynecoid, anthropoid, android, and platypelloid (see figure 1). Cynthia Ukah, explained that the gynecoid is the best for childbirth among the four. But what makes the gynecoid ideal for delivery?
Figure 1: Types of female pelvis. Click on image to enlarge.
Characteristics of the gynecoid pelvis
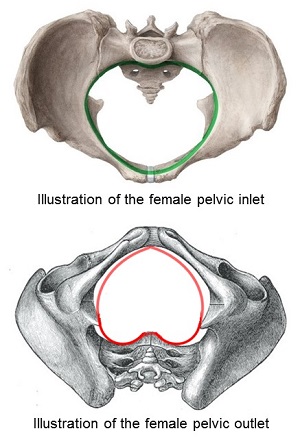
Figure 2: The female gynaecoid pelvic inlet and outlet (not drawn to scale). Click on image to epand.
Cultural beliefs and traditions in many parts of Africa contribute to some of the delays in seeking help during obstructed labour, increasing the risks that mothers and their unborn child face as a result of culturally based decisions.
In East Africa for example, a delayed delivery can be attributed to the promiscuous nature of the husband's wife; in this case, the midwife presses her to confess her crime. [5] While in Mozambique, adultery by the husband can also kill the pregnant woman, if the woman with whom he had sex approaches his wife while she is giving birth.
Another example can be found among the Esan people of Edo State, Nigeria. They generally believe that a woman is responsible for the health problems of her family, including her own, which are caused by violations of customs or traditions. They believe that obstructed labour is caused by sex in the afternoon or in the fields, adultery, or a woman taking her husband's belongings, such as money. According to this culture, her fortune will only turn around if she confesses. [5]
These beliefs cause what is known as phase 1 delay, in which the decision to seek medical care is postponed, exposing the mother and unborn child to an increased risk of complications and possibly death as a result of obstructed labour.
Many of the risk factors for obstructed labour are socio-economic and health system related. They include:
In a study conducted in Gombi local government in Adamawa state, Nigeria, 200 girls aged 15 to 24 who married before the age of 16 and had at least one child were interviewed using questionnaires. Data from this study revealed that 49% of respondents experienced obstructed labour during birth [7], compared to 1.5% in the general population. [8]
The pelvic bone, which is critical to a child's safe passage during delivery, does not fully mature until age 20 to 25, and the uterus, cervix, and other delivery organs may not be fully mature at this age, resulting in a high rate of obstructed labour among this group of women.
These figures are poor when compared with the combined ratio of 2.5 medical staff (i.e., (Doctors, Nurses and Midwives) per 1000 population estimated by the WHO in its 2016 World Health Report as being adequate for coverage of primary care interventions generally.
The critical health workforce shortage situation in Nigeria, when combined with ongoing brain drain of doctors and nurses in the country worsens healthcare provision.
But Nigeria is not alone. In 2022, the BBC reported for example that approximately 1,200 Ghanaians had migrated to the United Kingdom in search of higher paying jobs. Among those who migrated were the most senior and skilled nurses. [11]
Healthcare workforce shortages and brain drain creates a void, leaving citizens of affected African countries with insufficient and poorly trained health workers.
The direct causes of obstructed labour in African women can be discussed under two broad categories as follows:
I. Maternal factors include:
II. Fetal factors include:
Obstructed labour does not just appear and disappear; it usually leaves a trail of devastation for both the mother and child. One of the effects of obstructed labour is infection, i.e., the introduction of bacteria into the bloodstream (sepsis).
Melissa Dean; a midwife and founder of Casa Natal Birth and Wellness Center, explained in an interview that sepsis is typically caused by frequent and repeated cervical exams done throughout labour over many hours. This can introduce bacteria up into the cervix. She also stated that early opening of the waters can introduce bacteria into the system, particularly if labour has been delayed for several days, allowing bacteria to grow.
Other equally significant consequences of obstructed labour include:
1. Uterine rupture: Prolonged labour, multiple pregnancies, excessive uterine contraction especially when induced, previous uterine surgeries can all lead to uterine rupture in obstructed labour.
2. Urethral loss: The use of instruments to aid delivery can cause urethral trauma. Pressure exerted on the urethral by the big head of a baby can reduce blood to the organ and cause damage.
3. Fistula formations: These occurs when unnatural passageways are created as a result of obstructed labour among other causes, between the genital and urinary tracts (i.e., the womb (uterus) or vagina and the bladder - the organ in the body that holds urine before it's voided, or the urethra - the urine passage way for voiding).
It can also occur between the between genital and intestinal (bowel) tracts (i.e., the womb (uterus) or vagina and the rectum - the part of the bowel that holds poop (stool) before it's voided.
So, there are numerous types of fistula formations that may complicate obstructed labour. The two most common are known medically as vesicovaginal fistula (VVF) and rectovaginal fistula (RVF). In both cases, urine or poop dribbles through the vagina respectively to add more misery to the dangers associated with obstructed labour.
It has been estimated that between 30 - 130,000 women who give birth in sub-Saharan Africa annually have delivery-related fistula. [13]
4. Pelvic inflammatory disease: Prolonged labour, use of instruments, and early water break can contribute to this disease.
5. Cervical destruction: Excessive stretching of the cervix, prolonged pressure on it by the baby's head or body, infections, and trauma from the instruments used in aiding delivery all contribute to destroying the cervix during obstructed labour.
Melissa Dean warns that if no intervention is sought, the baby will more likely die as a result of stress over time. For the mother, she believes that infection and maternal exhaustion are the greatest risks of death for her.
Lack of oxygen, birth trauma, infections, premature separation of the placenta, and prolonged compression can all cause an infant to die as a result of obstructed labour. [14]
A child who survives obstructed labour could be left with deformities of the brain and other vital organs of the body while the mother’s reproductive organs such as the vaginal, cervix, uterine might be damaged beyond repairs.
Africa could learn and adopt some of the interventions that have improved the quality of childbirth in developed continents such as Europe and North America.
Given the several direct and indirect factors contributing to obstructed labour in Africa, several policy, and healthcare proposals that have been advanced for its reduction can be summarised as follows:
Malaysia has successfully reduced its maternal mortality ratio by 94%. In 1950, the maternal mortality ratio was 530 per 100,000 live births, but by 2009, it had dropped to 28. This was achieved as a result of massive investments in competency-based training for their healthcare providers. Furthermore, midwives were placed in rural areas with limited road access, advances in medicine and technology, improvements in the healthcare delivery system, the implementation of a risk-reduction strategy, and a confidential investigation into maternal deaths were all made. [15]
Traditional beliefs are so entrenched in African society that they have a negative effect on health. While having a set of beliefs is not wrong, those that impede people’s collective progress and survival should be discarded. Many nations around the world have overcome the scourge of obstructed labour through the integration of technology, improved healthcare facilities, and improved welfare provisions for healthcare providers; Africa can do the same if the political will is there.
Mothers and their unborn children have the right to safe and complications-free delivery and political will must be mustered to assure this right to them
1. Desta M, Mekonen Z, Alemu AA, Demelash M, Getaneh T, Bazezew Y, Kassa GM, Wakgari N. Determinants of obstructed labour and its adverse outcomes among women who gave birth in Hawassa University referral Hospital: A case-control study. PLoS One. 2022 Jun 24;17(6):e0268938. doi: 10.1371/journal.pone.0268938. Available from:here.
2. Girma T, Gezimu W, Demeke A. Prevalence, causes, and factors associated with obstructed labour among mothers who gave birth at public health facilities in Mojo Town, Central Ethiopia, 2019: A cross-sectional study. PLoS One. 2022 Sep 22;17(9):e0275170. doi: 10.1371/journal.pone.0275170. Available from:here.
3. World Health Organization (WHO). Managing prolonged and obstructed labour. Educational material for teachers of midwifery. Module 4 of Midwifery education module - 2nd edition. [Internet. 2008]. Cited July 2, 2024. Available from here.
4. Burgess MD, Lui F. Anatomy, Bony Pelvis and Lower Limb: Pelvic Bones. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from here.
5. Wall LL. Overcoming phase 1 delays: the critical component of obstetric fistula prevention programs in resource-poor countries. BMC Pregnancy Childbirth. 2012 Jul 18;12:68. doi: 10.1186/1471-2393-12-68. Available from here
8. Girls not brides. Child marriage. [internet,n.d] cited June 15, 2024. Available from here.
7. Adedokun O, Adeyemi O, Dauda C. Child marriage and maternal health risks among young mothers in Gombi, Adamawa State, Nigeria: implications for mortality, entitlements and freedoms. Afr Health Sci. 2016 Dec;16(4):986-999. doi: 10.4314/ahs.v16i4.15. Available from here.
8. Oguejiofor CB, Ezugwu CJ, Eleje GU, Emeka EA, Akabuike JC, Umeobika JC, Ogelle OM, Umeononihu OS, Eke AC. Emerging Predictors of Obstructed Labour in a Single Nigerian Centre Population of a Low Resource Setting. Trends Med Res. 2022;17(4):136-144. Epub 2022 Oct 1. Available from here.
9. Voice of Africa. Nigeria copes with a growing number of doctors, nurses. [internet, n.d]. Cited June 28, 2024. Available from here.
10. World Bank Group. World Health Organization's Global Health Workforce Statistics, OECD, supplemented by country data. 2003 - 2021. [Internet]. Cited. June 30 2024. Available from here.
11. BBC. Ghana patients in danger as nurses head for NHS in UK- medics. [internet, n.d] cited June 16, 2024. Available from here.
12. Fantu S, Segni H, Alemseged F. Incidence, causes and outcome of obstructed labour in jimma university specialized hospital. Ethiop J Health Sci. 2010 Nov;20(3):145-51. doi: 10.4314/ejhs.v20i3.69443. Available from here.
13. Hareru HE, Wtsadik DS, Ashenafi E, Debela BG, Lerango TL, Ewunie TM, Abebe M. Variability and awareness of obstetric fistula among women of reproductive age in sub-Saharan African countries: A systematic review and meta-analysis. Heliyon. 2023 Jul 22;9(8):e18126. doi: 10.1016/j.heliyon.2023.e18126. Available from here.
14. Collins KA, Popek E. Birth Injury: Birth Asphyxia and Birth Trauma. Acad Forensic Pathol. 2018 Dec;8(4):788-864. doi: 10.1177/1925362118821468. Available from here.
15. Norhayati MN, Nik Hazlina NH, Sulaiman Z, Azman MY. Severe maternal morbidity and near misses in tertiary hospitals, Kelantan, Malaysia: a cross-sectional study. BMC Public Health. 2016 Mar 5;16:229. doi: 10.1186/s12889-016-2895-2. PMID: 26944047; PMCID: PMC4779219. Available from here.
Related:
Why African women die more from birth-related bleeding
Social Factors Shaping African Women’s Health
6 Conditions that Put Pregnant African Women at Risk of Death
12 Top African Women's Health Issues and How to Take Action
Published: July 2, 2024
© 2024. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.