By: Elizabeth Obigwe, B.Sc. Anatomy. Freelance Writer. Medically reviewed by The DLHA Editorial Team.
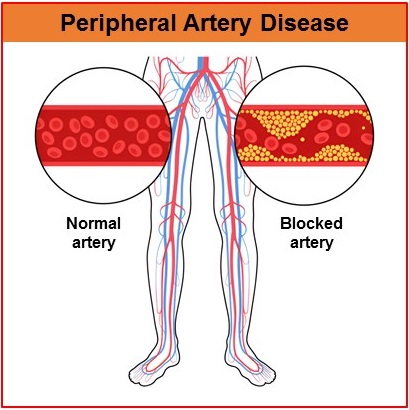
An illustration showing the difference between a normal artery and a blocked artery
Peripheral Artery Disease (PAD) is a condition where the arteries that carry blood to your legs, arms, or other parts of the body outside the heart and brain become narrowed or blocked. The narrowing of the artery is usually due to the buildup of a fatty substance called plaque.
This buildup makes it harder for blood to flow through the arteries, which can lead to pain, cramping, or weakness, especially in the legs when walking or exercising. Although it can occur in other parts of the body, PAD most commonly affects the legs
Peripheral artery disease is also called peripheral arterial disease. Some authors also refer to it as peripheral vascular disorder (PVD). However, PVD is a more encompassing term that includes conditions affecting other vessels in the body like veins and lymphatic vessels.
This article will discuss the causes, risk factors, symptoms and complications associated with PAD. Diagnostic tests, treatment and preventive measures for PAD will also be explained in detail.
There is a wide margin in the estimated prevalence of peripheral artery disease. PAD has an estimated prevalence of 4.5 to 57% globally [1] and 1.7% to 53% in sub-Saharan Africa. [2] These variations depend on the study and factors like study population and study design may influence results.
Nonetheless, about 73% of the global burden of PAD is found in low and middle-income countries (LMICs) with particularly high prevalence in sub-Saharan Africa [3].
Furthermore, PAD appears to be more common among women than men in the African population with a male-to-female ratio of 1:3-4 [1]. This means that for every man who is at risk of developing PAD, 3 or 4 women are equally at risk. However, this gender difference in prevalence is not as noticeable in high-income countries. [3]
Figure 1: An illustration showing the flow of blood in a normal artery and an artery blocked by cholesterol. Click on image to enlarge.
The most common cause of PAD is atherosclerosis. This is the thickening or hardening of the arteries caused by a buildup of fat, cholesterol, and other substances on the inner wall of an artery. This buildup is called plaque (See figure 1). The plaques in PAD form in the arteries of the arms or legs (most commonly legs), causing them to become narrow, thereby blocking the proper flow of blood.
Other less common causes of peripheral artery disease are [4, 5]:
Several factors, especially those that lead to the formation of plaques can increase your risk of developing PAD:
Studies have shown that older adults, especially those 65 and older are more likely to develop PAD. One study showed that while PAD had a prevalence of 4.3% among people older than 40 years, the prevalence among those older than 70 years was 14.5% [6]. However, the condition is generally more prevalent in a younger age group (45 to 49 years) in low-income countries than in high-income countries. [7]
Smokers are 4 times more likely to develop PAD compared to nonsmokers. In fact, half of all peripheral artery diseases can be attributed to smoking. They are also likely to experience an onset of symptoms almost a decade earlier and have a poorer survival rate.
Additionally, heavier smokers are more likely to develop PAD than light smokers and even former smokers have an increased risk of PAD compared to people who have never smoked. However, people who stop smoking are less likely to develop complications and have improved survival rates. [6, 8]
The risk of a diabetic patient developing PAD is similar to that of a smoker. However, PAD in diabetic patients is more likely to be asymptomatic due to co-existing nerve damage in a greater part of their limb. Also, experts say that diabetes mellitus is a stronger risk factor for PAD in women than in men. [6, 8]
Hyperlipidemia is a condition where there is a high level of fat (lipids) in the blood. The lipids that are likely to be present in the blood at elevated levels are cholesterol and triglycerides. The risk of PAD is increased by a high level of cholesterol in the blood, a condition known as hypercholesterolemia.
Hypertension is commonly known as high blood pressure. Studies show that as many as 50% to 92% of patients with PAD have hypertension. [6]
Having a family history of PAD or other vascular diseases like vasculitis, stroke, and heart disease can increase your chances of developing PAD. [7]
Patients with obesity, chronic kidney disease and metabolic syndrome have an increased risk of PAD.
Blacks are at higher risk of developing PAD compared to people of other races.
The feelings or complaints (symptoms) that you get to make your doctor to suspect that you have PAD, depends on the clinical stage or grouping of the disease. This grouping provides doctors with a structured way to assess how advanced the condition is. Each stage or classification corresponds to specific symptoms and their intensity.
PAD may not cause obvious symptoms in some people—up to 50% of general patients. Because of the absence of symptoms, this group of patients is the most under-recognised and undertreated with up to 70% of cases not known by the patient’s primary care physicians. [4]
Claudication is recognised as the classic symptom of PAD. It is an aching, discomfort, or burning in the muscles of the calves, thighs, or buttocks triggered by activity such as walking or exercise and relieved by rest. If properly managed, this symptom is likely to become stable and not worsen.
This category of symptoms involves one or more of the following:
ALI involves a sudden and rapid onset of one or more of the following:
These symptoms of ALI are known as the “six Ps” and they may not all be present at the same time.
For peripheral artery disease diagnosis, your doctor will start by receiving your complaints and asking you a few questions about your symptoms and medical history. They would next examine you physically paying attention to checking your pulses in the forearm and feet bilaterally. At the end of the physical examination, your doctor may recommend any of the tests below for further confirmation of the clinical diagnosis.
An illustration of how an ankle-brachial index is carried out. Click on image to enlarge.
This is a quick, painless and noninvasive test that compares the blood pressure in your ankle to the blood pressure in your arm. The doctor or nurse uses a regular blood pressure cuff and a special device called a Doppler to listen to the blood flow in your arteries (See figure 2).. If the blood pressure in your ankle is much lower than in your arm, it suggests that blood is having trouble flowing to your legs, which could mean you have PAD. The value of a normal ABI is 0.90 to 1.40. A lower value indicates reduced blood flow to the legs.
This test measures the blood flow in your legs and arms by checking the volume of blood pulses in your arteries. Blood pressure cuffs are placed around your legs and arms. The machine records how well your blood flows with each heartbeat. If the readings are low, it could indicate that your arteries are blocked or narrowed due to PAD.
The imaging techniques used for diagnosing peripheral artery disease are computed tomographic angiography (CTA), magnetic resonance angiography (MRA) and duplex arterial ultrasonography. The CTA and MRA techniques are similar to the more common computed tomography (CT) and magnetic resonance imaging (MRI) but they are specialised versions used specifically for looking at blood vessels. Also, they are used when urgency and accuracy are required such as if a patient has critical limb ischaemia (CLI).
This is a specialised type of CT scan that focuses specifically on the blood vessels. A contrast dye is injected into the bloodstream to make the blood vessels more visible. The resulting images clearly show any blockages or narrowing in the arteries.
This is a specialised type of MRI that focuses on blood vessels. Similar to CTA, a contrast dye may be injected into the blood to highlight the arteries and veins, allowing doctors to see any narrowing, blockages, or other abnormalities in the vessels.
Duplex arterial ultrasonography is a specialised type of ultrasound that combines regular ultrasound with Doppler ultrasound. It shows both the structure of your arteries and the blood flow through them. Unlike CTA and MRA, it does not require a contrast dye.
The physician moves a small handheld device over your skin. The screen shows detailed images of your arteries and the speed of the blood flow. If the flow is slow or blocked in certain areas, it suggests PAD.
Since the circulatory system is all connected, the impact of PAD can go beyond just the affected limb. People with atherosclerosis in their legs often experience it in other areas of their body as well. When the condition is left untreated or discovered late, it can lead to a number of complications. Some of these complications include: [9]
Peripheral artery disease treatments are aimed at managing the condition and slowing down progression. There is no cure for the disease yet. As such, treatment typically has two main goals:
Management begins with lifestyle modification to prevent disease progression. Then medical and interventional therapy are added to control symptoms and reduce the risk of cardiovascular events.
Risk factors modification for peripheral artery disease mostly includes lifestyle changes, some of which may be supervised for optimal results.
It has been shown that discontinuation of smoking or use of tobacco in any form decreases the rate of PAD progression and increases long-term survival. [6] If you cannot quit independently, you can ask about programs that can help you quit smoking.
If you are hypertensive, your doctor will administer an antihypertensive therapy to manage your blood pressure. Bringing blood pressure to less than 140/90 in nondiabetic and 130/80 in diabetic patients has been shown to improve outcomes. [6]
Statin therapy is used to lower blood cholesterol in patients with high levels of cholesterol. Besides its cholesterol-lowering effects, statin can also improve walking distance and speed in patients with PAD. [6]
If you are overweight, losing weight is beneficial in PAD management. You may be able to maintain better blood pressure and cholesterol when you maintain a healthy weight
You should eat more healthy meals such as fruits, vegetables, and whole grains. Reduce intake of saturated sodium, fats, added sugars, and alcohol.
Stress generally worsens health problems. Make efforts to minimise your stress which will in turn improve your sleep quality resulting in better emotional and physical health.
Exercise for peripheral artery disease needs to be performed regularly and the benefit may become noticeable after a few months. Your physician may recommend a supervised or home exercise program. The supervised programs usually take place in the hospital about 3 times a week for 3 to 9 months. It mostly involves treadmill walking but exercise for the upper body may also be recommended if needed.
The home program allows you to exercise within your home with some form of monitoring. You may be expected to take a 30 to 50-minute walk. [7]
Generally, exercise therapy involves walking until you reach your pain tolerance. You then stop for a brief rest and start walking again as soon as the pain resolves.
If you do not benefit sufficiently from risk factor modification and exercise programs, your doctor may prescribe some medications.
Cilostazol is usually prescribed for claudication. It is an antiplatelet medicine that prevents blood clotting and further narrowing of arteries. It improves your symptoms and makes walking easier.
In some cases, daily aspirin may also be prescribed.
If you do not respond to risk factor modifications, exercise programs and medication, your doctor may have to employ minimally invasive procedures like balloon angioplasty and stent placement (see figure 3). If this isn't equally effective, they may resort to surgical procedures like bypass grafts and endarterectomy. [10]
An illustration showing balloon angioplasty and stent placement. Click on image to enlarge.
Your doctor inserts a thin tube (catheter) with a small balloon at the tip into the blocked artery. Once in place, the balloon is inflated to push the plaque against the artery walls, widening the artery and improving blood flow. The balloon is then deflated and removed.
After a balloon angioplasty, a stent (a small mesh tube) may be left in the artery to keep it open. The stent supports the artery walls and prevents it from narrowing again, ensuring blood can flow more easily.
In this surgery, your doctor creates a new pathway for blood to flow around the blocked artery. They use a healthy blood vessel from another part of your body (or a synthetic tube) to "bypass" the blockage and restore normal blood flow to the affected area.
This is a surgical procedure where the doctor makes an incision in the artery and removes the plaque buildup directly from the artery walls. Once the plaque is removed, the artery is stitched up to restore proper blood flow.
If you are at risk of developing PAD, here are some preventive measures you can take.
PAD does not have a cure. So once you have been diagnosed with the condition, you will have to visit your doctor regularly for continuous monitoring and management. If caught early, the disease progression can be slowed down with the right treatment to prevent complications.
You will have to protect and take good care of your legs and feet to avoid injuries that can lead to ulcers. Do not go barefoot or wear tight shoes. Also, inspect your legs and feet regularly for any cuts, sores, redness or other abnormalities.
If you notice any foot problems, see your doctor immediately.
Peripheral Artery Disease (PAD) is a serious yet manageable condition that affects lots of people around the world and in Africa. It is a progressive disease, which means that it gets worse over time if left untreated. Early detection and treatment are critical in slowing the progression of the disease and preventing complications
Although there are some existing research studies on the disease, further research in sub-Saharan African countries is needed to better understand the burden and risk factor profile for PAD.
1. Mehta N, Ogendo S, Awori M. Prevalence, progression and associated risk factors of asymptomatic peripheral arterial disease. Annals of African Surgery. 2018;14(1). doi:10.4314/aas.v14i1.6. Available from here.
2. Johnston LE, Stewart BT, Yangni-Angate H, Veller M, Upchurch GR, Gyedu A, et al. Peripheral arterial disease in Sub-Saharan Africa[. JAMA Surgery. 2016;151(6):564. doi:10.1001/jamasurg.2016.0446. Available from here.
3. Beidelman ET, Rosenberg M, Wade AN, Crowther NJ, Kalbaugh CA. Prevalence of and risk factors for peripheral artery disease in rural South Africa: A Cross-Sectional Analysis of the HAALSI Cohort. Journal of the American Heart Association. 2024;13(1):e031780. doi.org/10.1161/JAHA.123.031780. Available from here.
4. Conte SM, Vale PR. Peripheral arterial disease. Heart, Lung and Circulation. 2018;27(4):427–32. doi:10.1016/j.hlc.2017.10.014. Available from here.
5. Kullo IJ, Rooke TW. Peripheral artery disease. New England Journal of Medicine. 2016;374(9):861–71. doi:10.1056/nejmcp1507631. Available from here.
6. Olin JW, Sealove BA. Peripheral artery disease: Current insight into the disease and its diagnosis and management. Mayo Clinic Proceedings. 2010;85(7):678–92. doi:10.4065/mcp.2010.0133. Available from here.
7. U.S. Department of Health and Human Services. Peripheral artery disease: Causes and risk factors [Internet]. National Heart, Lung, and Blood Institute. [Updated 2022 March]. Cited 2024 Sept 30. Available from here.
8. Morley RL, Sharma A, Horsch AD, Hinchliffe RJ. Peripheral artery disease. BMJ. 2018;360:j5842. doi:10.1136/bmj.j5842. Available from here.
9. Gul F, Janzer SF. Peripheral vascular disease [Internet]. StatPearls. [Updated 2023 Jun]. Available from here.
10. Zemaitis MR, Boll JM, Dreyer MA. Peripheral arterial disease [Internet]. StatPearls. [Updated 2023 May]. Available from here.
Published: September 27, 2024
© 2024. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.