Globally, self-medication is a common practice. It's particularly popular in Africa.
By: Victoria Iyeduala (Freelance Health and Wellness Writer)
Click on image to enlarge.
Introduction
Self-medication is the usage of drugs, herbs or home remedies on one’s own initiative, or on the advice of another person, without consulting an authorised health professional.
People often self-medicate as a first line of treatment for various symptoms like fever, pain, headache, cold and many other problems.
"There are some categories of medications people are permitted to self-medicate on, but oftentimes, this encourages them not to seek professional care", says Dr. Sadeeq Abdulsalam MD, MHE, Migration Health Physician, International Organisation for Migration, Lagos, Nigeria and former Medical Officer, Kano State Primary Healthcare Management Board, Kano State, Nigeria.
This article will discuss self-medication in Africa, focusing on prescription and non-prescription drugs, herbal medicine and home remedies.
It will explain:
According to a definition by the World Health Organization (WHO), “self-medication involves the use of medicinal products by the consumer to treat self-diagnosed disorders or symptoms, or the intermittent or continued use of medication prescribed by a physician for chronic or recurrent diseases or symptoms”.
When you self-medicate, you do three things:
The first part of self-medication is recognising the signs and symptoms you're experiencing and associating them with a particular illness.
You, your relatives, friends or an unauthorised health professional may be the ones to recognise these symptoms and connect them to an illness.
Self-diagnosis is often based on
Once you've diagnosed yourself with an illness, you get the medication you believe will treat the condition. The medication can be pharmaceutical drugs, herbal medicine or home remedies.
You may get the medicines because
"Self-medication means taking drugs on one's own initiative or on the advice of another person, without consulting a doctor or other authorised healthcare professionals", says Roseline Oluwatobi Akande (Pharmparrot), Pharmacist, Medplus Pharmacy, Ibadan, Nigeria
Since you got these drugs without a prescription from a doctor or an authorised health professional, you use them relying on your knowledge or intuition, how someone else used them or the instructions on the label.
Research indicates that self-treatment with medications is highly prevalent in African countries.
In two different Ethiopian studies published in 2018 and 2023 respectively, approximately 7 out of 10 study participants interviewed practised self-medication.
In a 2018 survey, nearly 1 in 2 Tanzanians reported that household members obtained medication without a prescription in the past year.
According to a 2020 study, 96% of 106 Egyptian patients interviewed were frequently self-medicating.
Also, a 2019 study in Eritrea revealed that 248 out of 313 students interviewed (i.e. 79%) practised self-medication.
A similar study in Nigeria found that 47.8% of participants practised self-medication.
Some health conditions, illnesses and symptoms Africans regularly self-medicate for are:
When you self-medicate responsibly, you use non-prescription drugs and use them correctly.
Responsible self-medication involves:
Responsible self-medication has many benefits, including:
Table 1: showing types of self-medication: responsible and irresponsible self-medication.
Click on image to enlarge.
The adverse effects of self-treatment with medicines are mainly a result of irresponsible self-medication.
Irresponsible self-medication medication is treating yourself with prescription drugs without a doctor's prescription.
Irresponsible self-medication also involves:
Irresponsible self-medication increases the risk and dangers of self-medication, such as:
Many reasons for self-medication have been identified over the years.
According to Pharmacist Akande, "The reasons behind self-medication are unique to everyone."
"Some are just understandably unwilling to submit to the inconvenience of visiting a doctor for what they rightly feel they can manage for themselves, given adequate information”, she added.
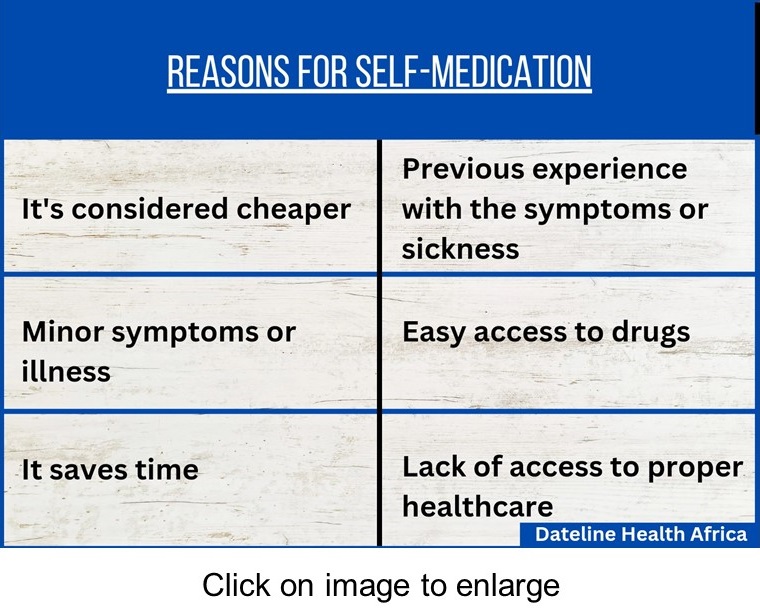 Africans self-medicate for several reasons including
Africans self-medicate for several reasons including
In most cases, self-medication costs less than getting treatment from a medical practitioner. Getting adequate hospital treatment in Africa is expensive, especially in private hospitals.
Factors like transportation costs if you live far away from public clinics, doctor consultations, tests and examinations, and treatment increase the cost of getting professional help.
According to Dr. Abdulsalam, seeing a doctor sometimes isn't very cheap. Sometimes the medication people need to get better is not so expensive.
When people consider all they will spend on getting professional treatment, they choose to go to the nearest pharmacy shop to get drugs they believe can cure their illness.
One of the main reasons people practise self-medication is because they or someone else they know has previously had a similar illness or symptoms and used the particular treatment.
People usually associate their current symptoms with a past illness that has similar symptoms. Therefore, they tend to use assumed effective medications in treating their illness.
It is common for people to self-medicate for an illness they consider to be minor or not life-threatening. This could be because the symptoms are not severe or go away when treated with common effective drugs that are easy to get.
Examples of illnesses usually considered to be mild are fever, cough and catarrh, uncomplicated malaria, stomach pain and headache.
People can easily get access to drugs in many African countries. Over-the-counter (OTC) or non-prescription, prescription-only, and herbal medications are easy to get in pharmacies, convenience stores, and online. Home remedies are made with household ingredients available in shops and markets.
In many African countries, Patent medicine or Chemist store owners frequently sell prescription drugs to customers without a prescription.
Many people have busy schedules that may not allow them to spend a lot of time trying to get access to treatment in hospitals.
Also, cases people consider emergencies may not be attended to on time in hospitals. This is because several things cause delays at hospitals.
For example, public health centres are usually congested most days. You can spend up to three to four hours at the hospital before speaking with a doctor.
Some can't even afford the time necessary to undergo tests and examinations or be on bed rest to recover fully.
Essential drugs are very important in healthcare. These drugs are used for common infections, diseases and health disorders.
They should be readily available to health professionals and patients in public clinics. However, sometimes these hospitals don't have these drugs in stock.
You could go to a public health centre, where a doctor prescribes drugs for you, but the pharmacy doesn’t have most of the drugs on the prescription.
Also, some public health centres can't offer proper treatment for some illnesses because of a lack of appropriate equipment and medical practitioners.
These problems are common in countries where healthcare is grossly inadequate for many reasons.
Pharmacist Akande advises, "You can consider self-medication only when you have adequate knowledge of the drug you want to take and can practise responsible self-medication."
"Self-medication is permitted with a particular category of drugs called non-prescription drugs. With non-prescription medication, you don't need a healthcare professional. They're for common ailments. You have a headache, and you take paracetamol (acetaminophen). You have a cough, and you take cough syrup", said Dr. Abdulsalam.
Dr. Abdulsalam also advises that you should try self-medication only if you're familiar with the dose, method of administration and indication for that medication.
Always remember that the use of herbal and home remedies is at the consumer’s risk. Therefore use with great caution.
Dr. Abdulsalam advises that you should avoid self-medicating with prescription drugs.
You shouldn't self-medicate if you can't correctly diagnose yourself with an illness. This could be because you're not familiar with the signs and symptoms or you don't have sufficient knowledge about the symptoms.
It's advisable to see a doctor instead of attempting self-medication with prescription drugs.
You should also shun self-medication when the symptoms are severe or life-threatening. In such situations, consult a doctor as soon as possible.
Drugs that Africans popularly self-medicate with are usually easy to get.
The following are common classes of these drugs:
Research shows that analgesics and antibiotics are the most commonly used drugs for practising self-medication.
According to this study, paracetamol (acetaminophen), an analgesic, was one of the most commonly used drugs for self-medication.
Analgesics, also called painkillers, are pain relieving drugs. People easily conclude that they need a pain relieving drug because they feel pain in a part or parts of their body. They're also commonly used for treating fever.
Examples of popular analgesics used are paracetamol (acetaminophen), ibuprofen and aspirin.
According to research, self-medication with antibiotics is alarmingly common in many African countries with the West African sub-region having the highest prevalence of misuse/abuse.
48.3%, 22.7%, 92.2%, and 43.1% of participants in different studies self-medicated with antibiotics.
Even though most antibiotics are prescription-only drugs, people have easy access to them. Antibiotic medications can be obtained without a prescription in many pharmacy shops in African countries.
Commonly misused or abused antibiotics are penicillin, tetracycline, ciprofloxacin, amoxicillin, ampicillin, ampicillin-cloxacillin (ampiclox), amoxicillin-clavulanic acid, erythromycin, azithromycin, chloramphenicol, cotrimoxazole, and metronidazole.
People use them when they feel or assume that they have infections or an illness that an antibiotic can cure.
Malaria is common in Africa and is treated with antimalarial medications. Antimalarial drugs are prescription drugs, but people frequently use them to self-medicate for symptoms assumed to be due to malaria.
A study in Nigeria showed that a little above 3 out of 10 participants self-medicated when they had malaria.
A small 2021 study also from Nigeria revealed that nearly 3 out of 10 people who self-medicated for COVID-19 used antimalarial drugs.
Artemisinin-based Combination Therapy (ACT) medicines like artemether-lumefantrine and artemether-amodiaquine, and chloroquine are the popularly used drugs.
Pharmacy shops in Nigeria stock loads of antimalarial drugs in different doses and brands and sell them to customers without prescription on a daily basis.
Because antimalarial drugs are easily accessible, people don't bother about going to see a doctor for malaria treatment and they go to a pharmacy instead to get drugs for themselves. They do this anytime they suspect they have malaria.
 WHO states that about 7 to 8 out of 10 Africans have used a form of traditional medicine as primary health care, with herbal treatment being the most common.
WHO states that about 7 to 8 out of 10 Africans have used a form of traditional medicine as primary health care, with herbal treatment being the most common.
A 2018 review indicates the use of alternative medicine, which includes herbal and home remedies, is high in Sub-Saharan Africa (SSA).
Results from a Nigeria-focused study showed that 1 of every 2 people who self-medicated used alternative medicine.
Home remedies are made with household items such as food items. This makes it common for people to use home remedies they made themselves or bought from someone else to treat common illnesses like malaria, skin problems and common cold.
Herbal medicines are easily accessible to the public and are common in African homes. They're advertised and sold openly in many African countries.
For example, herbal concoctions are usually hawked by women in Nigeria and are patronised by many. In Ghana, herbal treatments are frequently advertised on TV.
Herbal drugs are frequently used for common infections and diseases such as malaria, typhoid, hair and skin infections, diarrhoea, infertility, STIs, diabetes and hypertension.
Many antifungal drugs are non-prescription drugs and are available for sale in pharmacies and supermarkets. The most commonly used forms are creams and pills.
An example of antifungal drugs is ketoconazole, which is used to treat skin and hair infections.
Other commonly used drugs for self-medication are
Self-medication is prevalent in Africa and poses a huge public health problem as it is currently not well-regulated.
"Responsible self-medication should be optimised as it is an important and underused resource for healthcare and it provides an opportunity for collaboration and consultation among consumers, nurses, pharmacists and physicians", Pharmacist Akande suggests.
Some ways to promote responsible self-medication, prevent irresponsible self-medication and regulate the practice of self-medication are explained below.
The first step to regulating the practice of self-medication is by creating awareness at community, state and national levels around self-treatment and self-medication, its benefits, risks and dangers.
By creating awareness, people can learn how to practise self-medication responsibly and know when it is expedient to see a doctor.
Programs should be created to educate and sensitise owners of drug store outlets like pharmacies, chemists, and patent medicine stores, on best practice in the proper dispensing of prescription and non-prescription drugs to customers.
They can be taught how to advise customers and help increase their awareness about their symptoms and the drug they request for.
They can also learn how to handle customers asking for prescription-only drugs and harmful doses of medicines.
They should also be encouraged to have a pharmacist on hand to advise customers on drug use.
Health professionals should always interview patients thoroughly to ensure they're not practicing any form of self-medication that can affect their present treatment.
They should be mandated to encourage their patients to seek a doctor or qualified nurse's care for illnesses they may have self-medicated for but experience recurring symptoms.
They should also encourage their patients to practise only responsible self-medication and teach them what it is and how to do it.
Since pharmacists and nurses are more likely to be approached by people first, they should be encouraged to obtain the necessary advanced qualifications and license to prescribe prescription-only drugs.
The public health policies, regulations and laws that regulate the manufacture, importation, advertisement, sale, distribution and use of medications should be reviewed and updated periodically to bring them in line with best practices worldwide and subject to the peculiar health systems situation in each nation state in Africa.
Drug manufacturers should include information clearly indicating prescription-only and non-prescription drugs on the packaging. Also, instructions on labels should be clear and simple enough for patients to understand.
You're self-medicating if you treat yourself with drugs without advice or prescription from an authorised medical practitioner.
Self-medication is popular in Africa. It may be beneficial to the consumer when practised appropriately or responsibly. It may also cause health problems if practised inappropriately or irresponsibly.
Cost of treatment, delays in healthcare centres, lack of access to healthcare professionals and facilities, and past experience with sickness have been identified as a few reasons people practise self-medication in African countries.
Headaches, abdominal pain, malaria and typhoid fever are some illnesses people commonly self-medicate for, with painkillers, antibiotics and antimalarial drugs being the most widely used.
Responsible or appropriate self-medication contributes some benefits to primary health care and should be encouraged.
Irresponsible self-medication is harmful to the consumer and public health and should be discouraged.
With effective policies, regulatory enforcement of laws and awareness promotion, self-medication can be properly channeled in support of cost effective primary healthcare in Africa.
1. World Health Organization (WHO) (2000). Guidelines for the regulatory assessment of medicinal products for use in self-medication. PDF
2. Tadesse, Y. B., Kassaw, A. T., & Belachew, E. A. (2023, March 21). Evaluating self-medication practices in Ethiopia. Journal of Pharmaceutical Policy and Practice, 16(1).
3. Shafie, M., Eyasu, M., Muzeyin, K., Worku, Y., & Martín-Aragón, S. (2018, March 26). Prevalence and determinants of self-medication practice among selected households in Addis Ababa community. PLOS ONE, 13(3), e0194122.
4. Hertz, J. T., Madut, D. B., Tesha, R. A., William, G., Simmons, R. A., Galson, S. W., Maro, V. P., Crump, J. A., & Rubach, M. P. (2018, December 31). Self-medication with non-prescribed pharmaceutical agents in an area of low malaria transmission in northern Tanzania: a community-based survey. Transactions of the Royal Society of Tropical Medicine and Hygiene, 113(4), 183–188.
5. Zeid, W., Hamed, M., Mansour, N., & Diab, R. (2020, June 12). Prevalence and associated risk factors of self-medication among patients attending El-Mahsama family practice center, Ismailia, Egypt. Bulletin of the National Research Centre, 44(1).
6. Araia, Z. Z., Gebregziabher, N. K., & Mesfun, A. B. (2019, February 19). Self-medication practice and associated factors among students of Asmara College of Health Sciences, Eritrea: a cross sectional study. Journal of Pharmaceutical Policy and Practice, 12(1).
7. Akinnawo, E. O., Onisile, D. F., Alakija, O. A., & Akpunne, B. C. (2021, April 5). Self-Medication with Over-the-Counter and Prescription Drugs and Illness Behavior in Nigerian Artisans. International Journal of High Risk Behaviors and Addiction, 2021; 10(2):e107221.
8. WMA - the World Medical Association - WMA Statement on Self-medication. (2022, October 25). Retrieved March 28, 2023
9. Oyediran, O. O., Ayandiran, E. O., Olatubi, M. I., & Olabode, O. (2019). Awareness of risks associated with Self-medication among Patients attending General Out-patient Department of a Tertiary Hospital in South Western Nigeria. International Journal of Africa Nursing Sciences, 10, 110–115.
10. Kassa, T., Gedif, T., Andualem, T., & Aferu, T. (2022, January). Antibiotics self-medication practices among health care professionals in selected public hospitals of Addis Ababa, Ethiopia. Heliyon, 8(1), e08825.
11. Khalid, G. M., Jatau, A. I., Ibrahim, U. I., Dungus, F. M., Shitu, Z., Sha’aban, A., & Burji, S. L. (2019, January). Antibiotics self-medication among undergraduate pharmacy students in Northern Nigeria. Medicine Access @ Point of Care, 3, 239920261984684.
12. Ayana, H., Sileshi, T., Bule, M. H., & Chaka, E. E. (2021, December). Non-Prescription Antibiotics Use and Associated Factors Among Drug Retail Outlets in Ambo, Ethiopia: A Cross-Sectional Study. Patient Preference and Adherence, Volume 15, 2739–2747.
13. Egwu, C. O., Aloke, C., Chukwu, J., Nwankwo, J. C., Irem, C., Nwagu, K. E., Nwite, F., Agwu, A. O., Alum, E., Offor, C. E., & Obasi, N. A. (2023, January 3). Assessment of the Antimalarial Treatment Failure in Ebonyi State, Southeast Nigeria. Journal of Xenobiotics, 13(1), 16–26.
14. Wegbom, A. I., Edet, C. K., Raimi, O., Fagbamigbe, A. F., & Kiri, V. A. (2021, June 4). Self-Medication Practices and Associated Factors in the Prevention and/or Treatment of COVID-19 Virus: A Population-Based Survey in Nigeria. Frontiers in Public Health, 9.
15. Traditional Medicine. (2023, March 24). WHO | Regional Office for Africa. Retrieved March 28, 2023
16. James, P. B., Wardle, J., Steel, A., & Adams, J. (2018, October). Traditional, complementary and alternative medicine use in Sub-Saharan Africa: a systematic review. BMJ Global Health, 3(5), e000895.
17. Yeika, EV., Ingelbeen, B., Kemah, BL., Wirsiy, FS., Fomengia, JN., Marianne van der Sande, M. (2021): Comparative Assessment of the Prevalence, Practices and Factors Associated with Self-medication with Antibiotics in Africa: A Systematic Review and Meta-analysis. Tropical Medicine & International Health 26 (8); 862-881. doi:10.1111/tmi.13600
Self-medication in Africa: 4 commonly misused drug categories
Self-Medication in Africa: What are the consequences?
Published: April 4, 2023
Updated: May 17, 2023.
© 2023. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content without alteration or modification and subject to attribution as to source.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.