The treatment of sleep disorders may be quite complex and often require multiple professionals and options.
In treating your sleep disorders, your doctor may choose one or a combination of the following options:
Lifestyle and sleep hygiene modifications
These consist of:
Behaviour Therapy
This is a treatment approach that is designed to help change some of the day-to-day behaviors that may be contributing to your sleep disorder. It is probably the best long term option for the management of chronic sleep problems.
Behaviour therapy requires seeing a psychologist or psychiatrist or a behavioural sleep psychologist, as available.
The process of behaviour therapy may be expensive as it takes quite a while to see significant and sustained results.
There are very few specialists in many African countries today that are trained and licensed to practice in the field of clinical behaviour therapy.
The use of sleeping medications in the treatment of sleep disorders should be limited to the short-term (i.e., few days to one or two weeks).
This is because sleep medications have moderate to severe side effects, and do cause dependency and tolerance.
When considered necessary, your doctor may prescribe specific medication(s) to you depending on the type of sleep disorder that you are diagnosed with.
For example, if you are diagnosed with:
These drugs are best used for a duration of one to few weeks in the management of acute or transient insomnia.
The goal of treatment is to normalize disrupted sleep pattern in the short term while switching to behaviour therapy for the long term management of chronic insomnia.
Examples of antidepressants in common usage in Africa include:
Many unregulated dietary supplements and herbal preparations are available for purchase in most African pharmacies, supermarkets and chemists. Your allopathic doctor my not readily recommend or prescribe their use because of lack of evidence on their safety and efficacy.
Your doctor may also recommend non-pharmaceutical therapies for you like:
This is aimed at training the insomnia patient to re-associate the bed and bedroom with sleep and to re-establish a consistent sleep-wake schedule. It is a form of behaviour therapy.
The training will include;
The following limitations of non-pharmacological management have been identified from research studies with respect to insomnia:
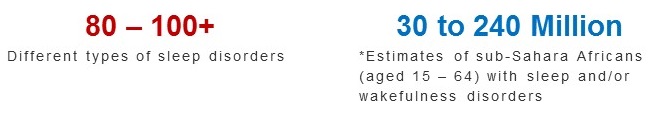
There are like 80 to over 100 different conditions that make up sleep disorders. These are grouped into two; i.e. Dyssomnia or Parasomnia.
The three commonest sleep disorders globally are in the dyssomnia group and include Insomnia, Sleep apnea and Restless leg syndrome.
Due to the pressures and circumstances of daily living, you like many others worldwide may have occasional trouble falling asleep, staying asleep, and having refreshing and satisfying sleep. This does not necessarily mean that you suffer from sleep disorder.
If you think that you may have a sleep disorder, speak early with your doctor or other healthcare provider in order to be professionally evaluated, diagnosed and treated appropriately for return to better sleep quality and sustenance of quality health.
Do not self-medicate yourself for a perceived sleep disorder.
Also do not use dietary supplements and herbs without talking with your doctor or pharmacist.
Normal Sleep: What African should know
Slideshow: Who is at risk of major sleep disturbances?
Sleep medications: Types, Uses and Side effects
Published: February 7, 2023
© 2023. Datelinehealth Africa Inc.
Permission is given to copy, use and share content freely for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.