By: Dr. Azuka Ezeike, MBBS, FWACS (Obstetrics and Gynaecology), FMCOG, MSc (Public Health). Medically reviewed by: A. Odutola, B.Med.Sci., MBBS, PhD, FRCSEd.
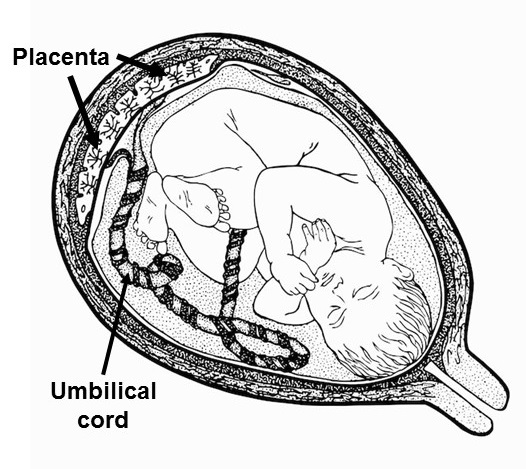
Baby (foestus) in the womb and connected to the placenta by the umbilical cord. Image credit: dnbr from Freepik
Imagine a temporary organ, designed specifically for your pregnancy that works relentlessly to nourish and protect your baby. That’s the placenta. The placenta is often referred to as ‘the tree of life’. This is because of the critical role it plays in sustaining the baby during pregnancy.
The placenta is an organ that provides nutrients and other requirements to your baby. Though the development starts early in pregnancy, it becomes fully developed and functional around the 12th week.
A normal placenta is a spongy round or oval-shaped structure measuring about 22 cm in diameter. It is about 2.5 cm thick and averagely weighs a little over a pound (500 grams). [1] It contains many segments known as cotyledons. There are about 15-20 cotyledons in a mature placenta. The umbilical cord connects the placenta to the baby.
This article discusses the development of the placenta, its functions, importance in pregnancy, and the various abnormalities that can arise. It also highlights how these abnormalities are managed for a healthy and successful pregnancy outcome.
After fertilisation of the egg by the sperm, the embryo is formed. This undergoes multiple divisions into many cells. The cells are of two groups: the inner and outer cell mass. The inner cell mass develops into the baby while the outer cell mass forms the chorion frondosum.
The chorioic frundosum consists of trophoblasts and the extraembryonic mesoderm and is surrounded by chorionic villi that send finger-like projections into the basal decidua, which is in the endometrium or inner lining of the womb (uterus). The chorion frondosum forms the major part of the implanted placenta.
The trophoblasts are of two types:
The syncytiotrophoblast is the part of the trophoblast that makes contact with the lining of the womb (endometrium). In pregnancy, the endometrium is known as the decidua. The cytotrophoblast lies below the syncytiotrophoblast.
The placenta is developed from the cytotrophoblast, syncytiotrophoblast and another part of the developing fetus (baby) called the extraembryonic mesoderm. [2] The amniotic sac develops alongside the placenta and later fuses with the decidua. The mother's blood flows through blood vessels called the spiral arteries into a space called the intervillous space in the placenta. In this space, the mother's blood bathes the baby's blood vessels in the tertiary villi. This allows for the exchange of oxygen and nutrients. Under normal circumstances, there is no mixture of the mother’s and baby’s blood.
The trophoblast produces the hormone Human Chorionic Gonadotrophin (HCG) in the early stages before the placenta becomes fully formed. The fully formed placenta produces progesterone which is the major hormone of pregnancy.
The placenta is the lifeline between you and your baby as it is crucial for the growth and development of the developing baby (fetus). It provides all the essential nutrients for the baby so the baby cannot survive without it. The proper development and function of the placenta are necessary for a successful pregnancy.
The placenta performs vital roles in supporting your pregnancy.
The functions include:
The placenta functions as the lungs of your baby. It is responsible for the transfer of oxygen and carbon dioxide. The mother's blood is rich in oxygen while the blood coming from the baby is poor in oxygen and rich in carbon dioxide. The umbilical arteries (blood vessels in the baby) carry the oxygen-poor blood from the baby to the placenta while the mother’s spiral arteries carry oxygen-rich blood to the placenta.
At the placenta, your blood takes up carbon dioxide from the baby's blood and gives up oxygen. Your baby’s blood releases carbon dioxide and takes up oxygen. The oxygen-rich blood is carried to your baby’s organs through the umbilical veins. This transfer of gases across the placenta happens by a process called simple diffusion.
The placental provides the medium for the transfer of many nutrients. These include:
Glucose
The baby has limited capacity to produce glucose (sugar). Therefore, the main source of glucose is the mother. The transfer of glucose across the placenta occurs mainly through facilitated diffusion, a type of transport mechanism.
Amino acids
Amino acids are the building blocks of protein. They are very essential for the production of protein in the baby. They are transferred across the placenta by a process known as active transport. Sometimes the transfer of amino acids occurs along with the transfer of electrolytes like sodium.
Fatty acids
Fatty acids play a critical role in the synthesis of some important compounds in the baby. These compounds include prostaglandins and phospholipids. The transfer occurs mainly through simple diffusion.
Water, electrolytes and vitamins
The placenta also serves as a medium for the transfer of water, vitamins and electrolytes. Water, sodium and chloride ions are mainly transferred through simple diffusion. Calcium and vitamins are transferred through active transport.
The placenta is a hormone-producing organ. Its hormone-producing function is essential for the support of the pregnancy.
The hormones produced by the placenta include:
The placenta produces this hormone at the early stages of development. The hormone is released in the mother's blood and urine and can be used to detect the presence of the pregnancy.
Human Placental Lactogen
This is also called Human Chorionic Somatomammotropin (HCS). This hormone helps in maintaining enough blood sugar in the mother to enable transfer to the baby. It is also involved in breast development in preparation for breastfeeding.
From around the 12th week of pregnancy, the placenta produces oestrogen and progesterone. The oestrogen helps in the growth of the womb and the breasts. Progesterone helps to prevent contractions of the womb muscles, thus preventing premature labour.
Some antibodies are large and cannot cross the placenta. However, some smaller antibodies like IgG can cross the placenta. This is important to note in women with some immune-related diseases like Grave’s disease. The transfer of antibodies across the placenta can adversely affect the unborn baby. The antibodies are transferred through a process known as pinocytosis.
Most drugs can cross the placenta. This can be beneficial or harmful. The benefits include the use of some drugs like steroids to help the baby’s lungs mature. Some drugs can however be harmful when transferred to the baby as they cause damage to the organs. This risk of damage is higher in the first three months of pregnancy. The drugs are usually transferred through simple diffusion, facilitated diffusion, active transport and pinocytosis.
The placenta protects the baby by serving as a barrier to the transfer of some drugs, harmful molecules and infections from the mother. [3] It also performs an excretory function by helping to remove wastes like carbon dioxide.
Watch the video below to learn more about the functions of the placenta.
Video: Functions of the placenta. Click on image to watch.
Placental problems result from abnormalities in:
Some of these include [1, 4]:
Illustration showing complete placenta praevia (type 4). Image Credit. Click on image to enlarge.
The normal site of implantation of the placenta is the upper or middle part of the womb (fundus). Placenta praevia is when the placenta implants wholly or partly in the lower segment of the womb.
The cause is unknown, but possible risk factors are discussed later.
The severity can range from type 1 in which the placenta encroaches to the opening of the cervix (mouth of the womb) to type 4 in which the placenta completely covers the cervical opening.
The condition is associated with painless bleeding from the vagina in the last three months of pregnancy. [5] This bleeding can be severe enough to lead to the death of the mother or the baby.
Illustration showing placenta abruption. Image Credit. Click on image to enlarge.
Placental abruption (also known as placenta abruptio) is when a placenta that is in a normal location in the womb separates before labour starts. This usually happens in the last three months of pregnancy.
The cause is often unknown. Injury from fall or in a car accident during pregnancy may be a factor. Other risk factors include; previous history of abruption, water break before 37 weeks of pregnancy, and others discussed later.
Placenta abruption is characterised by bleeding from the vagina (in some instances) and pain in the abdomen. This can lead to complications for the mother and baby.
Illustration showing placenta accreta. Image Credit. Click on image to enlarge.
Placenta accreta (also known as Placenta Accreta Spectrum, PAS) is the abnormal attachment of the placenta to the womb uterus). The normal placenta has a separation plane between it and the lining of the womb. This allows for easy removal.
In placenta accreta, the placenta invades into and sometimes even beyond the muscles of the womb. It is also known as the morbidly adherent placenta.
Placenta accreta leads to retained placenta, bleeding after delivery, longer hospital stay post-delivery. It may also lead to maternal death.
Battledore placenta is when the umbilical cord is inserted at or near the margin of the placenta, rather than at the centre. It is associated with preterm labour and abnormality in the baby’s heart rate.
In the circumvallate placenta, the baby’s side of the placenta is smaller than the mother’s side. This makes the membranes fold around the edge of the placenta making the central part of the placenta look exposed. This abnormality is associated with premature breakage of the water, placental abruption and preterm labour.
This is when the placenta has an accessory (additional) lobe. This lobe is attached to the main placenta by blood vessels originating from the baby. This increases the risk of vasa praevia. Vasa previa is a rare condition where the baby’s blood vessels cross or run near the internal opening of the cervix. Succenturiate placenta can also result in the retention of the additional lobe after delivery.
This is when the placenta has two equal lobes. The lobes are separated by a membrane with the umbilical cord inserted into either of the lobes.
Other minor forms of placental structural abnormalities exist.
Placental insufficiency refers to a condition where the placenta does not function properly, leading to an inadequate supply of oxygen and nutrients to the baby. This can result in poor growth of the baby. Placental insufficiency can be caused by various factors, including high blood pressure, diabetes, and smoking.
Several factors can increase the risk of placental abnormalities. These include:
Some placental problems may not be noticeable till delivery, especially in locations where ultrasound is not readily available.
However, abnormalities in the placenta may be associated with symptoms like:
Others include
Any of these abnormalities should prompt you to see your doctor. To confirm the diagnosis, your doctor would check you and do some tests like an ultrasound.
While some placental abnormalities may not lead to problems in pregnancy, some others may lead to harm to you or your baby.
Risks to the mother
Risks to the baby
Findings from history and examination and images (pictures) obtained through Ultrasound and Magnetic Resonance Imaging (MRI) would help your doctor detect problems with the placenta.
Your doctor uses the history of the symptoms and the findings on examination to differentiate between one type of abnormality or the other. This is very useful in differentiating placenta praevia from placental abruption.
Placental problems are usually detected with ultrasound. The use of ultrasound shows the site and structure of the placenta. The blood vessels running through the placenta can be checked with a Doppler ultrasound, a special type of ultrasound technique. This helps in diagnosing placenta insufficiency and conditions like vasa praevia.
Magnetic resonance Imaging (MRI) is a type of test that is useful in diagnosing morbidly adherent placenta.
The management of placental abnormalities depends on the type and severity of the condition, as well as the stage of pregnancy.
Some general approaches for the management of abnormalities of the placenta include:
Close Monitoring: Having a placental abnormality increases the risk of pregnancy. This requires more frequent antenatal visits and ultrasounds to monitor your health and that of your baby. There may also be a need for admission in some cases.
Bed Rest: If you have placenta praevia, your doctor will admit you for bed rest. This can help minimise the chances of preterm labour or excessive bleeding. The bleeding in placenta praevia is usually unpredictable. Bed rest at the hospital keeps you close to allow for early intervention
Medications: Some placental abnormalities increase the risk of premature delivery. Medications like steroids are usually prescribed to hasten the maturity of the baby’s lungs.
Delivery Planning: Conditions like placenta accreta will require planning of the delivery beforehand. This is because delivery may require a caesarean section, or even a hysterectomy (removal of the womb) in severe cases.
In some placental abnormalities like placental abruption, early delivery may be necessary to preserve the health of the mother and baby.
Surgical Intervention: Conditions like placenta accreta, placenta praevia and abruption of the placenta require surgical intervention. This could range from caesarean section to other procedures like hysterectomy, in severe cases.
The placenta is a critical organ that is central to supporting a healthy pregnancy. Its functions, from providing nutrients and oxygen to protecting the fetus, are essential for the development and well-being of the baby. When there are placental abnormalities it can pose significant risks to both the mother and the baby.
The advent of ultrasound has reduced the complications due to abnormal placenta. These problems could be detected on time and interventions instituted to prevent adverse effects. Regular antenatal care is key to ensuring a healthy pregnancy and a safe delivery for you and your baby.
1. Rathbun KM, Hildebrand JP. Placenta abnormalities. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Last updated October 17, 2022. [Cited 2024 Aug 27]. Available from here.
2. Herrick EJ, Bordoni B. Embryology, placenta. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Last updated: May 1, 2023. [Cited 2024 Aug 27]. Available from here.
3. Gude NM, Roberts CT, Kalionis B, King RG. Growth and function of the normal human placenta. Thromb Res. 2004;114(5–6):397–407. doi: 10.1016/j.thromres.2004.06.038. Available from here.
4. Jansen CHJR, Kastelein AW, Kleinrouweler CE, Van Leeuwen E, De Jong KH, Pajkrt E, et al. Development of placental abnormalities in location and anatomy. Acta Obstet Gynecol Scand. 2020 Aug 28];99(8):983–93. doi: 10.1111/aogs.13834. Available from here.
5. NHS.UK. What complications can affect the placenta? [Internet]. Last reviewed August 22, 2022. [Cited 2024 Aug 29]. Available from here.
Published: December 28, 2024
© 2024. Datelinehealth Africa Inc. All rights reserved.
Permission is given to copy, use and share content for non-commercial purposes without alteration or modification and subject to source attribution.
DATELINEHEALTH AFRICA INC., is a digital publisher for informational and educational purposes and does not offer personal medical care and advice. If you have a medical problem needing routine or emergency attention, call your doctor or local emergency services immediately, or visit the nearest emergency room or the nearest hospital. You should consult your professional healthcare provider before starting any nutrition, diet, exercise, fitness, medical or wellness program mentioned or referenced in the DatelinehealthAfrica website. Click here for more disclaimer notice.